| Atrioventricular nodal branch | |
|---|---|
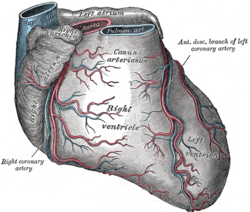 Sternocostal surface of heart. | |
 ARTERIES: RCA = right coronary AB = atrial branches SANB = sinuatrial nodal RMA = right marginal LCA = left coronary CB = circumflex branch LAD/AIB = anterior interventricular LMA = left marginal PIA/PDA = posterior descending AVN = atrioventricular nodal VEINS: SCV = small cardiac ACV = anterior cardiac AIV/GCV = great cardiac MCV = middle cardiac CS = coronary sinus | |
| Details | |
| Identifiers | |
| Latin | ramus nodi atrioventricularis |
| TA98 | A12.2.03.110 A12.2.03.213 |
| TA2 | 4140 |
| FMA | 3851 |
| Anatomical terminology | |
The atrioventricular nodal branch is a coronary artery that supplies arterial blood to the atrioventricular node, which is responsible for initiating muscular contraction of the ventricles. The AV nodal branch is most often a branch of the right coronary artery.
YouTube Encyclopedic
-
1/3Views:555 46154 7711 568 991
-
Atrioventricular reentrant tachycardia (AVRT) & AV nodal reentrant tachycardia (AVNRT)
-
AV Nodal Reentry Tachycardia (AVNRT) on ECG / EKG
-
Electrical Conduction System of the Heart Cardiac | SA Node, AV Node, Bundle of His
Transcription
Atrioventricular Re-entrant Tachycardia is also known as AVRT for short. And it's a type of supraventricular tachycardia where you have an abnormal loop of electricity, or a re-entrant circuit, going around and around between two pathways. So you have to have two pathways, one being normal AV conduction system, so that's one of the pathways. And the other pathway is an accessory pathway. And that's just an extra pathway that exists between the atrium and the ventricle. And atrioventricular re-entrant tachycardia. So I'm just going to erase this real quick, cause we're gonna re-draw that in a second. So normally, signal goes from the SA node through the atrium, to the AV node. And remember, the AV node is sort of like the gatekeeper, or the bridge that bridges signal from the atrium to the ventricle. So in a normal heart, signal has to go through this AV node. And it goes through the AV node and down to the ventricles and causes ventricular stimulation and contraction. Sometimes there's an abnormal path, or an accessory pathway, which is an extra pathway between the atrium and the ventricle. So it could be here, it could be over here, I just drew over here for convenience. But there's this extra pathway. And signal can travel from the atrium to the ventricle through this pathway and excite ventricular tissue that way. Signal can also go from the ventricles through the atrium through this accessory pathway. So it can either go forward, or in the anterograde direction, which is from the atrium to the ventricle, or backwards, which is the retrograde direction. From the ventricles to the atrium. And the direction that it goes depends on a couple of things. It depends on the timing of the refractory period of the accessory pathway. And the refractory period, remember, that's the window of time right after a group of cells are excited, in which they can't be excited again. It's kind of like a recovery period. So say you sprinted 100 meters. You're not gonna be ready to sprint another 100 meters unless you take a little break. So the refractory period is sort of like a mini-recovery period. And again, whether or not the signal goes in this forward direction or this backwards direction depends on the timing of the refractory period of the accessory pathway, as well as the direction from which signal is coming towards this accessory pathway. So if you have normal conduction through the AV node, and you have an accessory pathway, this can set you up to have a re-entrant circuit, or this abnormal loop electrical activity going around and around and around, which could cause a tachyarrhythmia. So again, you need to have both a working AV conduction system and this accessory pathway in order to have AVRT. I think one of the best ways to better conceptualize AVRT is by going through the most classic example of AVRT, which is Wolff-Parkinson-White syndrome. So again, Wolff-Parkinson-White syndrome is a classic example of AVRT. And sometimes it's called WPW for short. So again, in Wolff-Parkinson-White syndrome, you have this extra pathway or accessory pathway that exists between the atrium and the ventricle. And you have signal that goes from the SA node to the AV node, and then to the ventricles and that signal can also go from the SA node through this accessory pathway and can stimulate the ventricles that way. So you're getting ventricular stimulation through the AV node and through this accessory pathway. Now something to note is that the AV node has special tissue that actually slows down conduction so when signal hits the AV node, the conduction slows down. However, this accessory pathway is just kind of like a hole between the atrium and the ventricle. It's not gonna slow down any signal. So the signal going from the atrium to the ventricle through this pathway is actually going to stimulate ventricular cells sooner than it would the AV node, cause this AV node has this built-in mechanism that slows down conduction. So you're going to see some changes on the EKG. You're going to see a shortened PR interval, and you're gonna see the slow rise in the slope of the QRS. Again, you have this shortened PR interval, the PR interval is usually less than 0.12 seconds. And that's because you have this pre-excited ventricular tissue that's getting stimulated before the normal conduction system has a chance to stimulate ventricular tissue. And because you're getting ventricular stimulation over a longer period of time, you're gonna have this slow rise in your QRS. This slow rise is called a Delta wave. And again, this is classic for WPW. Now it's important to note that this here is not AVRT. You're not gonna get a tachyarrhythmia just from this. However, in the event that you have a premature beat coming from the SA node going to the AV node, and if this accessory pathway happens to be in a refractory period, meaning that the signal isn't gonna travel this way through the accessory pathway, then you're gonna have signal going down through the ventricles. It's gonna travel back up. And by the time it reaches the accessory pathway, it will no longer be in a refractory period. So the signal can actually travel through the accessory pathway and then go back and stimulate the AV node. This creates the re-entry circuit. So you're gonna have the signal going around and around and around and around. And this is gonna create the tachyarrhythmia that you get in AVRT. Atrioventricular Nodal Re-entrant Tachycardia is another type of re-entrant tachycardia like AVRT, but it has its differences. So people call this AVNRT for short. Remember, this is very different than AVRT. It's called AVNRT, N is for Nodal, because the abnormal loop of electricity, or that abnormal re-entrant circuit, directly involves the AV node. And the tissue right around it. There is no accessory pathway in AVNRT. So again, this is the AV node, and here I drew a bigger AV node. I kind of blew it up. So this is the AV node, and the His Bundle, and the conduction system going down into the ventricles. So in AVNRT, there are two pathways that run through the AV node. There's a slow pathway, where an impulse travels more slowly down the path, and there's a fast pathway where the impulse can zip through. Now I'm gonna erase this real quick, cause we're gonna re-draw these in a second. Okay, something else to note. Just because of this inherent make up, the slow pathway has a shorter refractory period. Now remember the refractory period is that window of time when cells can't be excited again after they've already been excited. Whereas the fast pathway has a longer refractory period. I'm gonna abbreviate refractory period RP. Refractory period. So again: slow pathway, short refractory period. Fast pathway, long refractory period. So a signal comes down, and it's gonna split. And it's gonna rush down the fast pathway, reach this common final pathway, and then spread to the ventricles. Meanwhile, it's gonna slowly go down the slow pathway. After this impulse has been transmitted through this fast pathway, it's gonna go through the refractory period. So these lines through it mean refractory period. By the time the slow pathway signal makes it to the final common pathway, it's gonna hit the refractory period of the fast pathway, and it's gonna terminate. Because no signal can be activated this way since it's in refractory period. This slow pathway is gonna enter its own refractory period, a shorter refractory period. So it's actually gonna recover. And then the fast will recover. And both the slow and fast pathway are ready for business again. They're ready for another impulse. Now let's say that there's an early beat, or a premature beat that comes in. Sometimes people call these extra beats. So there's an early beat that comes in. And let's say it comes in at a time when the fast track is still recovering from a refractory period, but the slow track has already recovered from its refractory period and is open. So this beat's gonna send impulse down the slow track. As the slow track slowly makes its way down the slow track, the fast track is gonna recover from its refractory period. So by the time the impulse reaches this final common pathway, it's gonna send signal down. And because the fast track has recovered from its refractory period, this impulse can activate the fast track and send signal back up. If the slow track has already been through its refractory period and recovered from that refractory period, it can activate the slow pathway. And send signal back down. And what happens is, the impulse will continue to circle around and around. You're creating this re-entrant loop. And as it circles around and around and around, it's gonna keep sending signal down this way. So this loop is sending signal through the AV node at a much faster rate than a normal pace maker's would, so you might see a heart rate between 100 to even 250 beats per minute. And again, it's because you have this abnormal re-entrant loop, sending signal around and around and around which is gonna spit off signal down to the ventricles at a much faster rate than a normal pacer's would. EKG is gonna look like a supraventricular tachycardia where you have a narrow QRS complex, meaning it's less than 0.12 seconds or three small boxes. And you're gonna have a heart rate of greater than or equal to 100 beats per minute. Because that's what a tachycardia is. It's greater than 100 beats per minute. So on this EKG here, you can appreciate a narrow QRS complex, and again the QRS complex is narrow because there's normal activation of the His Purkinje system, and you notice that the heart rate is greater than 100 beats per minute. So the heart rate here is somewhere between 150 and 300 beats per minute. By looking from here to here, you can tell that the heart rate is above 100 beats per minute. So this is definitely a tachycardia.
Structure
Origin
The atrioventricular nodal branch sees significant variation in origin:
- proximal posterolateral branch from the right coronary artery in around 77%.[1]
- distal posterolateral branch from the right coronary artery in around 2%.[1]
- distal right coronary artery in around 10%.[1]
- right posterior interventricular artery in around 7%.[1]
- distal circumflex branch of left coronary artery in around 4%.[1]
The right coronary artery supplies the atrioventricular node in around 90% of people.[1][2]
In approximately 2% of people, the vascular supply to the atrioventricular node arises from both the right coronary artery and the left circumflex branch.[3]
Function
The atrioventricular nodal branch supplies the atrioventricular node, allowing for excitation of the ventricles.[1]
See also
References
- ^ a b c d e f g Kawashima, Tomokazu; Sato, Fumi (2018-10-15). "Clarifying the anatomy of the atrioventricular node artery". International Journal of Cardiology. 269: 158–164. doi:10.1016/j.ijcard.2018.07.022. ISSN 0167-5273. PMID 30001947. S2CID 51618750.
- ^ Mahadevan, Vishy (2012-01-01). "Anatomy of the heart". Surgery (Oxford). Cardiothoracic I. 30 (1): 5–8. doi:10.1016/j.mpsur.2011.10.011. ISSN 0263-9319.
- ^ Sow ML, Ndoye JM, Lo EA. The artery of the atrioventricular node: an anatomic study based on 38 injection-dissections. Surg Radiol Anat 1996;18:183–187
