Direct thrombin inhibitors (DTIs) are a class of anticoagulant drugs that can be used to prevent and treat embolisms and blood clots caused by various diseases. They inhibit thrombin, a serine protease which affects the coagulation cascade in many ways. DTIs have undergone rapid development since the 90's. With technological advances in genetic engineering the production of recombinant hirudin was made possible which opened the door to this new group of drugs. Before the use of DTIs the therapy and prophylaxis for anticoagulation had stayed the same for over 50 years with the use of heparin derivatives and warfarin which have some well known disadvantages. DTIs are still under development, but the research focus has shifted towards factor Xa inhibitors, or even dual thrombin and fXa inhibitors that have a broader mechanism of action by both inhibiting factor IIa (thrombin) and Xa. A recent review of patents and literature on thrombin inhibitors has demonstrated that the development of allosteric and multi-mechanism inhibitors might lead the way to a safer anticoagulant.[1]
YouTube Encyclopedic
-
1/2Views:9 680989
-
Applications of Genetic Tools to Clinical and Translational Research
-
2014 Scientific Sessions Presidential Address
Transcription
[Dr. Thomas Pearson] One of the real questions is how do we apply these marvelous new genetic tools in our research? And I guess one perspective is that if you want to look forward in terms of use of this, it's probably -- medicine isn't the right place to look forward, look at that, because the whole genetics revolution has already had a major impact on human health, and it's probably been through nutrition. If you look at the rice yields, this year, we're looking at the largest rice crop in the world -- yield in the world. And obviously, we're going to need it, given the commodities issues, but a variety of things having to do with plant genetics, et cetera. Just to give you a little introduction, my own experience of this is this is TAProots, this is my vineyard in upstate New York. I have a vineyard on Keuka Lake, which is one of the Finger Lakes, which grows most of the wine in upstate New York. And some of my grapes are these. These are good old concord grapes. These are American grapes. Nobody's been fiddling with these. These are Native American grapes. But you don't see a whole lot of bottles of concord wine on the shelf, at least not any more, and ours goes to grape juice, Welch's grape juice. And so those haven't been fiddled with, but if you're going to go into something more interesting, there are these -- all sorts of gene products. And most of that comes from the Cornell Experimental Station, which is in Geneva, New York, which is about 10 miles from my vineyard. And I like to go over there and watch them fiddle around with their grapes, which is practical genetics. And these are French varietals, which are bred for cold hardiness, tannin structure, all sorts of things, and you can kind of pick out. So if you're into agriculture, you know that genetics has already had a huge impact and provides us with beautiful products. These are some seedless grapes, which are table grapes. They're obviously crossbreeds of crossbreeds of crossbreeds of crossbreeds. So genetics has already had a huge impact on human health, but we're into medicine and the clinical sides of things. So what I wanted to talk about was talk a little bit, in finishing here, about some of the inferences we can make, that gene variants are causal for a disease, and kind of switching from what the usual evidence we want in epidemiology to the new context of the results of the tools we have, kind of a translation of those results, the inferences we make in epidemiology to the tools we have in genetics, then really talk about personalized medicine a little bit. A lot of places are starting personalized medicine programs. And obviously, many of these are based on genetic tools. This obviously is a whole course, but I want to just touch on two issues, genetic screening and pharmacogenetics, and then talk a little bit about, very briefly, some application -- further application of some genetic tools to research and experimental studies. Well, I think the first thing that struck me as I retooled in genetics and took the Bar Harbor course and read in my various textbooks, et cetera, is that genome-wide association studies have -- and the whole genetic genomic revolution already has had a tremendous impact on basic science. And one of the comments on Teri's last lecture was that as you go and look as these genome-wide association studies, I'd ask you how many epidemiology lectures have you seen recently, which right in the middle of the results will have a cell expression study or a histopathology analysis or a knockout model, mouse model in the middle of what, in essence, is an epidemiology study. I just -- it just -- this just totally blew me away. And they're the functional studies that Teri was talking about; they're very appropriate there. And so, to some extent, this is reverse translation. Talking about translational science and going from bench to bedside. Well, this is actually going from population, with the genome-wide models back to say, "What is this?" You've got this SNP in the middle of a gene desert. Okay, folks, go out and find out what's going on here. And that -- the message is not to other epidemiologists, oftentimes; it's back to our basic genetic scientists. So this is -- I was asking a -- or somebody asked the audience in a conference one day, "Tell me one thing that population science has done for the basic scientist." Well, I got up to the microphone and basically said, "Well, here it is. Here is a whole lot of work for a whole lot of people of insights that we didn't have before." So this whole insight's in the genome structure and function. You can see that just in the matter of a few years, the interest in some of these introns and regulatory elements obviously has sparked a -- has renewed interest sparked in them. These novel mechanisms of disease obviously are -- these insights that we actually probably know very little about how diseases occur. From some of these come proteins, as such, therapeutics, particularly in the area of clotting. But obviously, some of these have been cloned proteins, and these are useful. And then the other thing, of course, was that as we come up with these novel mechanisms of disease, you have new drug targets. You find another receptor, another enzyme, another -- and I've been very impressed with these ability to mass screen small molecule inhibitors where you can come up with a gene and then just run through hundreds of thousands of small proteins and get some hits to ones which will inhibit that receptor, et cetera, and then go on to animal work, Phase I. And so the rapidity and the magnitude of this is just mind-boggling. But certainly, the fuel for this are going to be these novel drug targets which obviously deal with novel mechanisms of disease. So if you -- I think some of Eric Lander and some of the visionary people in this kind of cringe a little bit when you try to pin them down about how genome-wide association studies have affected clinical medicine. But no one is arguing about how much they have really opened our insights into basic science. But I'm a little bit more optimistic than that. So you're all familiar with the surgeon general's criteria. And so what I thought might be interesting in this kind of summary way is to say we're reading all of these genome-wide association studies, how can we be sure, and the same way, how can we be sure that a behavior or a physiologic measure or a laboratory measurement has to do with causality, and you are all familiar with this. But let's look at each of these in the context of the genome association issues and maybe make some comments. Well, Teri's already mentioned, they say, "Well, the gene's there, the temporal relationship's not an issue." And I guess that's true. But there obviously is a subgroup of individuals who are also interested in expression of the gene, not just its presence in the genome, but it's expression, these expression arrays and a variety of things. And this is a temporal issue, because what this suggests is that the disease occurs during which time a disease is not quiescent. It's being expressed, and it's active. And so even this temporal relationship, obviously, I think could have some opportunities for studies which are looking at not only that the gene is present, but it's being expressed. And some of the functional studies that have been talked about deal with that. It's that these are expressed in the tissue of the interest, for example. I wanted to comment on the strength of association again. The nice question came up before. But what you have is multiple SNPs and other gene variants, and they all add to risk. And one of the real questions is, what is the composite risk of all the variants, known or unknown? And Teri showed a little bit about how those might be explained. But I wondered if -- well, then we're going to talk a little bit about dose responses also relevant here. And in this context, it would be the number of alleles, in other words, non heterozygous, homozygous for the susceptibility risk. So you can do dose response within this, obviously, and recessive versus dominant. One of the things I have been thinking about was just to do some back-of-the-envelope scratching out about this idea that was discussed about why you get such small odds ratios. And let's just do a little hypothetical study of 2,000 smokers -- a case-control study with, say, 2,000 smokers and 2,000 -- I'm sorry, 2,000 people with a disease and 2,000 people without disease. So whatever disease you'd like, cancer, heart disease, whatever. And when do you the odds ratios, of course you get an odds ratio of 2.25. And so this looks at the entire exposure by cigarette smoking. But let's -- what would you think if, in fact, you weren't smart enough to do all that together? And, in fact, you had to dice this up into individual exposures within the same class? Let's assume that 10 percent of individuals smoke Camel cigarettes, and all you can do is measure Camel cigarettes. Well, here what you see is 10 percent of the individuals are smokers. The denominator is not, "Do not smoke." It's, "Do not smoke Camels." Okay? And in this instance, then you get a much smaller odds ratio. And less than half as strong, really, in terms of risk above one. And I think this is what's happening in many ways, not even talking about gene-gene associations. But if, in fact, you put together Marlboros and Winstons and Kents and all the other coffin nails that we could come up with, you would be able to add all those together and come up with such. And I think that's just, in plain terms, kind of an illustration of what we're doing in trying to put all of these risks together. And again, I think we may not know all of the culprits in this area, but just to try to put it into something that could be a little bit more quantitatively understandable. This is just this illustration of the alleles. Here is risks -- genes associated with the breast cancer in the study by Easton. Here is the odds ratio per allele. And if you look within the data, the odds ratio associated with being heterozygous for these risk alleles or homozygous for this, you can see obviously there is this dose response, perhaps not so impressively down here. But the point is that I think one can fulfill what we like to see, of course, in our studies as some dose response, although the dominant and recessive issues, I think, become more complicated. We just had an electron replication of finding. And I don't want to say more than that other than that the genetics community, and particularly Steve Chanock and Teri's leadership, I think, have been quite much more militant about requiring these replications than the epidemiology communities had in its previous studies. And I think this has been a very positive response to this alpha error issue. The biologic plausibility, of course, you just heard what this is about, are the functional studies about why this could be occurring, and these are an important part. One wonders if one needs in vivo studies, some of the knockout or knock-in models would be -- at what point -- what are the standards of functional studies? You know, there's -- you'll see tremendous heterogeneity. Some of them will be essentially a bibliographic look at gene location and possibly expression. Others will get into some of the other much more convincing issues of actually gene product measurement and tissue expression and animal models. So I haven't seen a lot about kind of the -- what would be your minimum requirements. The consideration of alternate explanations, obviously, some of these models are very complex. And so when one finds an association, one wonders how these all fit together. This attribution of genetic risk I think would be one approach to say, well, if we can understand much of the heritability or the familial association, we would get an idea that we've identified all of the parts of these complex models. And I think we're still a way from it. So this whole heterogeneity -- obviously, I've shown this slide before in terms of the possible explanations and mechanisms of heterogeneity. And I think these, we need to keep in mind. The various cites, of course, many of the GWAS studies have looked at SNPs related to exons and introns. But the whole area of regulatory elements and how these things interact on a single gene basis, to say nothing about a multi-gene basis, obviously is part of the complexity that -- and so these alternate explanations, unfortunately, are virtually infinite. This is the Easton study again. And as part of that analysis -- actually, this is the second Easton paper, which specifically, I think, was looking at this issue of additional familial risks. So the point they were making is it's a known breast cancer loci, such as a BRCA, and such genes really only explain 25 percent or less of familial risk of breast cancer. There could be environmental and obviously, but in general, looking at the family histories of breast cancer and the risk that that imparts, only, what, 25 percent of that could be explained by the known genetic markers. So what they did was a two-stage study, which essentially excluded individuals with these markers. Forty-four hundred cases, 4,300 controls, and within the replication of SNPs in these huge numbers of cases of controls, and found these five novel loci related to breast cancer at 10 to the minus seventh. And these novel loci then identify the additional 3.6 percent of risk, so again, possibly on top of that 25 percent. But just to give you an idea of the complexity and the things ahead, they also noted in one of those Q-Q plots that Teri showed you, is that there were 1,792 additional SNPs associated at the P less than .05 level where there are only about 343 expected, suggesting about 450 additional SNPs in excess that would appear to be having something to do with susceptibility and maybe having a role in the complex nature. So this whole idea of alternate explanations and the ability to account for familial risk, I think, is something that's going to continue to be a challenge. This issue of cessation of exposure is interesting. Obviously, this knock-in and knockout, this gene replacement therapy is not a topic I'm going to get into. Obviously it has its own levels of controversy. But we do have a number of interventions which replace defective gene products, to suggest that -- and I'm going to give you one from Dr. Collins' laboratory, but certainly familial hypercholesterolemia, for example, heterozygous FH, we've been working on this for a while, in essence of up-regulating the LDL receptor to make up for the one that doesn't work. But I think we're going to see more with the insights of the receptors and the drug targets that they offer us, we're going to be seeing a lot more of this. And there's several exciting ones rumbling around in the development stage. The consistency with other knowledge obviously has to do with functional evidence again, et cetera, and animal models. And then finally, the specificity of association, obviously, was kind of based on one gene, one protein. But even that, I think, is being shaken a little bit by now a couple of examples. And I'll show you one of the shared association of diseases with gene variants in which you would appear to have one variant which isn't related to two different diseases. And so this specificity, which is one of the lower-ranked levels of causative evidence may, in fact, not be so causative. This is from Dr. Francis Collins' lab. It's in the "New England Journal," a paper published recently on this progeria syndrome. You've probably seen cases of this. These are children who are born and undergo an accelerated aging process to the point that they die of cardiovascular disease, interestingly to the drop out of cells in their arterial media by about the age of 13 years. So obviously, a severe disease. And now the defect has been found with modern genomic tools. It's this substitution of one glycine to the next in a codon, which has been basically a cryptic splice donor that produces an abnormal protein. This obviously gets to be kind of an unusual mechanism and variant that leads to this abnormal protein Lamin A, which has to do with a chunk of it missing so that it cannot release from a tether site on the nuclear membrane and then as the cell tries to transcribe proteins. This alters transcription and the widespread growth failure, et cetera. The idea here was, then, okay, now we've got a gene and a gene target, and once you understand all of these things, which this "New England Journal" paper describes, then what you have is the opportunity to fill with some of the gene products and what's going on downstream. And basically, in animal models and in cell models, inhibition of this enzyme prevents this anchoring of this abnormal protein, which then thereafter can't release and buggers up the cells. So what essentially, as Dr. Collins describes this, this goes in from some of this descriptive work and some of this functional work, rapidly into an open-label clinical trial of an inhibiter of this to see if they can get these children to start growing. It just illustrates the idea of once you understand the gene targets and then can survey for these small molecules that will be able to affect those gene targets, the opportunities that have never -- we've never had before of really doing something that otherwise we would have said it's just an untreatable genetic disease. And I think that's part of the excitement of the whole thing. There's a number, there's a subgroup of the Marfan syndrome, which has a similar kind of thing with actually a commonly available anti-hypertensive drug as the drug. So a lot of things that just really aren't so far-fetched, even though this is pretty complicated stuff. This is one of these studies which kind of looks at the specificity of this association of this SNP. And this particularly confers risk for prostate cancer, but it looks like it's protective of type 2 diabetes. And again, there may be questions that arise about how this single SNP could be doing this. But in fact, within the same study done in Iceland and then replicated in a larger group of patients here, you see the cases and controls, quite a substantial number of cases, controls. There's an odds ratio of 1.2, highly significant as a causative, as a susceptibility factor for prostate cancer. But then within the same study, again, once you have your genes done in a group, you can do cases, controls for a number of conditions. And here you have, for type 2 diabetes, case control studies, you have an odds ratio significantly less than 1, protective of type 2 diabetes. And in fact, there apparently, I didn't know about it, but apparently, there is literature which shows an inverse relationship in populations of prostate cancer in type 2 diabetics. But to some extent, the insight of that was -- was heightened by this potential genetic basis for that. So some of the specificity of these genes may not be particularly having to do with their mechanism of action. Let's talk a little bit about personalized medicine. This is a very popular term, probably means different things to different people. But at least to the boss at the NHGRI, it means that personalized medicine refers to using information about a person's genetic makeup to tailor strategies for detection, treatment and prevention of disease. And I think most of us who think about personalized medicine think about the human genome and the use of genetic markers, each person's personalized individual signature that would have impact on the approach to their prevention, diagnosis and treatment of disease on, again, a very individualized basis. The -- one of the things that has been pointed out is that family history starts out -- is perhaps the first step of a personalized medicine program, and unfortunately, we're not so good at taking family histories. A book on Teri's and my shelf is "Physical Diagnosis" by DeGowin and DeGowin. And if you look in that book, there's nothing on taking a family history at all. It just isn't in the book on how to take a history, and so maybe we shouldn't be surprised. The other thing is that once a proband occurs in the midst, it doesn't look like we're very good on acting about it at all. And this is a study I did with a medical student a while back. We had 5,620 consecutive patients admitted to 53 randomly selected hospitals around the country. Everybody had a standard criteria for coronary disease on entry. And when we reviewed these 5,620 discharge plans, only 37 of them, 0.7 percent, identified a plan to screen the first-degree relatives. And it actually didn't matter if the person was 35 with their heart attack or 75 with their heart attack, this wasn't part of anybody's plan. And we followed these folks up to six months after discharge. And only about one out of six children had ever been screened regardless of the risk or risk factors in the proband. So as we look at screening for genetic factors, I might say, "Well, why don't we do the things like asking, 'Has your mother, father, sister, brother had heart disease?' first, before we do all the heart disease genes for which we have no evidence that we're actually doing, okay?" Because we really aren't getting it there, so that the family history is part of this. So, you know, it's like, you know, it's right there. What are the -- what is the question? This is another rendition of a slide already shown by Teri. You know, this is -- this is a person at genetic risk on, you know, a cow, with it's -- what is the question? So we should do that. Now, one of the efforts, and Alan Guttmacher of the NCRI is one of the leaders of this, is a multi-agency initiative in the health and human services. It's the -- my -- the U.S. Surgeon General's Family History Initiative. And one of them -- one of the parts of this is My Family Health Portrait. It's a Web-based tool to collect and organize family history and information. I've given you the website. You can actually get a printout to share with your health care provider. So from the previous slide, kind of saying, okay, if you're not going to collect it, I'll collect it, and maybe you could do something about it. And of course, Thanksgiving day here in late November is -- has been for the last several years, the National Family History Day. So while you're sitting around carving up your turkey, you should be drawing a genotype, a pedigree on your wall or something and encourage Americans to talk about, write it down, health problems that run in their family. So the point is that I think this is really the first step. And we're going to talk about some of the evidence there is, that is the U.S. population or the U.S. health care population -- health care providers really ready for some of the genetic and genomic information currently available commercially? And I think most of us would agree, and there's been multiple editorials from multiple sources, is that we're probably not. And there's a whole group at NHGRI that work on the many issues here. Well, the other point of it is, to say that genetic screening is something new is actually not really correct because, of course, there has been newborn screening for some years. This is not necessarily DNA screening, some of this should probably be followed up with DNA screening. But we have been screening for genetic diseases for some time. By far, the most common is congenital hearing loss, but you can see a variety of others. And so we have been screening and putting into action the genetic counseling and the follow-up of these children for a long time. So there really is a precedent and something to build on. And obviously, some of these experiences, we need to take forward. So an effective screening program obviously needs to have analytic validity. That is, that we know what we're measuring, and there's good reproducibility. It's a clinical validity in terms of it measuring what we want to measure. Obviously, these are a variety of issues with some of their genomic ones. But I really want to talk about clinical utility as we roll things out, some of the genomic quality issues Teri's already covered up here. The condition should be frequent enough to justify the cost of screening, detection should be otherwise not -- detection would not otherwise occur at an early enough stage to perhaps prevent disease. Early treatment prevents morbidity. Treatments available and family and personnel are available to perform the screening and formulate results and institute the treatment. So the whole point is that we, in terms of the application to genetic markers to clinical practice -- and this is from a Greg Feero from the NHGRI and one of the other members in the office of the director in this editorial recently in JAMA obviously identifies four barriers to really carrying this out. The first is really lack of information about how these prevalence and how the prevalence and risk contribution markers varies across populations. We have a lot of data in Europeans, perhaps North Americans, et cetera, but other population groups obviously may have very different risk. And certainly, we have plenty of examples where the prevalence of a gene or its impact on disease varies tremendously from one population to the next. We have limited data on how the inheritance of multiple markers affects an individual's risk. We just talked about that, this whole gene-gene interaction, et cetera, and so this whole risk assessment quality. There's little information about how most genetic receptors interact with environmental factors. Again, the gene-environment issue, and then finally, there may be most desperate in terms of our research needs are that fewer studies -- few studies in common diseases have tested the effect of these interventions on genetic risk factors, really, again, identifying those markers, identifying the targets for drugs and going ahead and testing them. One of the issues we've had a lot of discussions and the Northwestern faculty have, Dr. Greenland and Lloyd Jones and others, have commented on some of the biomarker issues, as is very appropriate to do. But one of the points is you can look at a genome marker as just a new biomarker test. And so you'll have patients at risk for disease, you can take people at general risk or perhaps people at high risk of family histories, et cetera. But one of the real keys at the end of the day is to show that this is cost effective. And the number of studies on any biomarker, I don't care what it is, be it an imaging test or a serum marker or a gene marker, there are very few studies which use randomized designs in which the new test then would reclassify individuals in low and high risk and treat them accordingly and look for the outcome and compare whether or not with usual care in which this marker wasn't used, they just went ahead with treatment or no treatments, see what happens. If you look at the literature, there is very few of those. And one of the reasons there's very few of those is that from a commercial standpoint, once you develop a marker and are able to sell it, you have very little interest in this kind of a study, because all the study could do is actually show low cost effectiveness and actually be a commercial disincentive for its use. So I think this is a place for governmental funding, when we really need to know this kind of cost effectiveness research. And I think the genome markers would fit in these as well. Well, I wish I had a Larson cartoon about the elephant out of the barn, but it certainly is. I've taken off all the commercial names of this. But this is from a recent piece in JAMA about screening. But there, you can -- obviously a variety of direct consumer genetic testings are available, certainly The Whole Genome, 23 and Me, several companies. And these are complex risk screenings based on SNPs discovered through their ongoing research. You can also get singular or multiple trait testing for conditions for specific diseases using proprietary panels. There is obviously some studies available for paternity and family relationships, particularly using mitochondrial and Y chromosome panels. And there is some others, there is even some that you can get to tell you which diet to use. And so many of these are available, and so what's going to be increasingly happening is that, if you are a practitioner, someone is going to come with a printout of the polymorphisms that you have -- that your patient has. And you're going to be basically asked, "So what do I do now?" And obviously, this is going to not be -- because we're already quite obvious that many of the simple family screenings of taking, say, a blood pressure in the child of a hypertensive patient not being done, wait until you get to this level of complexity. And so there's been a variety of issues about this. So here we are, this is us. We're almost free. We've all figured out the genomics. We're about to -- oops. I think it's only about to get more complicated. And I think there is going to be a flood. Now, having said that, there obviously are some examples of genetic markers which have been, I think, considered and used. These are the lifetime risks for cancer of the breasts, of the ovary of these two BRCA markers. And you can see there are substantial lifetimes risks of some very bad, bad diseases. And so the natural history of this particular marker is well worked out. Unfortunately -- and this is from Wiley Burke, from the Jackson Lab course -- obviously points out that relatively little of the total incidents of breast cancer, unfortunately, is identified by the BRCA1 and 2 testing. And so the fallback position would be really to testify the affected relatives with breast or ovarian cancer. And then if she were positive, offer to affected relatives. This is not -- this is not an inconsequential cost. And I'm wondering if these are going to be coming down, if you can get your whole genome for $1,000. But anyway -- and obviously, there are some things you could do about it: prophylactic surgery, oophorectomy and mastectomy, tamoxifen, which may only be effective in some of the groups, and obviously a much more attentive look at breast cancer screening, maybe using breast MRI. So there are some examples to lead our way in terms of our approach to this, so I don't think it's all just hopelessness. This review by Schweiner [phonetic sp] really looked at the delivery of genomic medicine for chronic diseases currently in the literature. There were essentially three or four areas: outcomes of genetic services, consumer information needs and barriers to integrations. The key findings were really modest positive effects on anxiety, improvement, reduction of anxiety with the results of screening, mixed results on behavior change in terms of people, say, following up with screening recommendations, et cetera, very few studies with clinical outcomes. In terms of the clinical information needs, some, I think, very convincing evidence that there are low levels of genetics knowledge. But basically positive attitudes toward genetic testing, but some great concern of the inadequacy of the primary care work force to provide the counseling and referral, et cetera. In terms of barriers to integrations, there had been some concern about the oversight of this testing, how this testing was going to be done and the quality of it. So, many of our lab certification issues, I think, can address it, and there's considerable concern about the use of these data, the privacy and, in the case of positive finding, discrimination of that person against them. And so this is kind of what's out in terms of the use of genetic services and identify some of the issues we would have in terms of translating these into care. One of the positive steps forward is the Genetic Information Non-Discrimination Act, which is on the president's desk. And if he weren't marrying daughters, apparently would have been signed already. This was -- I think the primary author on the House side of this was actually my congresswoman, Louise Slaughter from our district in New York. And this really is a necessary building block because one of -- as you have seen, one of the literature -- the study's results identifies concerns about the discrimination if you do have your studies, genetic studies done, and this law then fixes the problem at least in the areas of health insurance and employment. So it prohibits health insurers from either requesting or requiring genetic information on individuals or their family members or using it for decisions on coverages, rates, et cetera. And this includes individuals who get genetic testing as part of research studies. So for those of us in research, it obviously, has this important part as well. And it also prohibits employers from requesting or requiring information or using it in decisions regarding hiring, firing, in terms of employment. Now, there are still many other issues involved, but certainly, I think this has been in the works for 10 years, right, Teri? [Dr. Teri Manolio] Twelve years. [Dr. Thomas Pearson] Twelve years? Yeah, so it's been in -- but it like passed 490 to five in the House, and I think there was only one senator that voted against it, and I didn't understand that. So apparently, this will be a law, and obviously is a step forward for the implementing and the practical aspects of genetic screening. I want to just say a couple things about pharmacogenetics. This field is the study of the differences in drug response to the allelic variation in genes affecting drug metabolism, efficacy and toxicity. It's an enormous -- it's a course in itself. But just to say we know there's a number of the aspects of drug metabolism that are under genetic control, particularly having to do with the systems that break down drugs, and the allelic variations then being either the normal metabolizers, the poor metabolizers in which the gene product doesn't break down the drug as much or a fast metabolizers in which you're forced to try to keep up, maybe have to use a higher dose to get the same blood level or therapeutic level. So there's obviously plenty to suggest that genes are very important here. And we know that there's tremendous heterogeneity across populations. These are -- if you're into tuberculosis control, the slow acetylator phenotype, looking at INH metabolism, obviously varies tremendously across populations, so that, for example, INH in this group could be a problem of not breaking down the drugs. And, in fact, non-supervised INH, the classic studies in Baltimore in the 1950s, unsupervised INH use turned out to be somewhat of a public health disaster as people with this high prevalence of slow acetylation obviously ended up with liver failure having to do with drug toxicity. You might also say that, in other populations, that this would not be a problem, and maybe in some populations might even be a reason for needing higher doses of this, with the Inuits, the Alaskan natives, et cetera, having a higher tuberculosis rate, at least in the days before drug resistant TB and AIDS. So the point is there's a lot of variability. These are the five studies in the GWAS collection so far, or at least in the first 109 GWAS that dealt with pharmacogenetics just to make the point that the GWAS certainly are a very reasonable tool for looking at this issue, again in an agnostic, non-hypothesis driven. Two of them have to do with nicotine, comparing this whole issue of nicotine dependency versus nondependent and how nicotine would really -- its method of action, really. One we referred to already by this Byum I think is one of the better studies, response versus no response in multiple sclerosis therapy to a beta interferon. This direct thrombin inhibiter was really a drug toxicity study but could be a model for many other hepatotoxicity studies. And then this methamphetamine dependence, again, another study of addiction versus control. So just the point is that even within the GWAS literature, there's a number of genome-wide association studies looking at drug-related issues. Really, finally, I want to just -- in terms of a comment relative to research, the genome-wide association studies now have a policy at NIH in terms of data sharing. And I think it's been alluded to before is that once you do the whole genome, there may be the opportunity to study many different phenotypes. And this should be a repository of great national importance so that other investigators may look at the issues involved. So the goal of this policy was to make available the genotype and phenotype databases as rapidly as possible to a wide range of scientific investigators. It includes depositing the data at the National Center for Biotechnology Information and in the dbGaP registry that we talked about. Obviously, plans of data submission and protection and obviously the lack of identification of information, personal information, how to access the data, the publication of results, and there's some statements on intellectual policy within that policy as well. And I think the driver of this really has been this open access, which has really been a tremendously consistent theme at the National Human Genomics Research Institute. It really has been. And it goes into many other suggested GWAS, but this high kind of opening up the idea that the human genome really isn't a commercial product. Let me tell you a story about this open access issue. I was at the Bar Harbor course on human genetics. And one of the things you could do during that time is see patients; you had a patient day. And I am a cardiologist. And so a couple other cardiology professors and I saw a patient. And she was a tall, slim person with long arms, et cetera. And her doctor, obviously, was interested. There was an "aneurysm" history in a parent. And obviously, the question was, did this woman have Marfan syndrome? In fact, there are criteria, major and minor criteria, for Marfan. She had one of the major criteria; you need two. And she had about, for like five of the other criteria, just a little bit below. So she didn't quite make all the classic criteria for Marfans. And so the decision was, well, why don't we just go do her genotype? Well, the genotype was $2,500. And we actually calculated the time from when the patent on the genotype would expire and how much it would cost us to echocardiogram her every year and treat it with beta-blockers. It was far cheaper to do it that way than to get this gene test because of the commercialization of this. And obviously, what we'd like to do is to say that this -- the technologies and the tests should be patented, and this is intellectual property. But the gene itself should not be something that one could control its use, that this should be available to all of us in medicine and in public health for the use of the public's good. And I think all of us were just a little peeved by this whole thing, that this was really a barrier to using science as we'd like to. So that's just a little personal vignette. But -- and the GWAS policy on open access on these data are available is, I think, part of that philosophy. And so for you investigators who might want to request and receive these data, you need to submit a subscription -- description of proposed research project. Obviously, this is a scientific research issue; this is not for commercial use or other uses. You submit a data access request, and it's cosigned by your institutional official. Obviously, if there is some commitments to protect data confidentiality, theoretically, the genome is the ultimate personal identifier, isn't it? There's really only one of them. And so theoretically, this is -- could be abusable. But there are many provisions in here to protect this confidentiality and to ensure they have security measures. If there are any problems here, to notify the data access committee about policy violations, and then to provide annual reports. So I think for our graduate students, et cetera, you know, we may not have the exact genome-wide association study in our own institution. But with this policy provides opportunities for many, many investigators, both trainees and established investigators, to be more active. So I just want to conclude saying this evidence for the causal associations, I think, is still in formative stages. The whole gene polymorphisms obviously have a little bit different wrinkles to them, but still, I think fit well within the usual epidemiologic constructs for causality. The application of products of genomics includes susceptibility assessment and pharmacogenomics. Obviously, I think these are some of the low-hanging fruit that still have some barriers as we have described. Unfortunately, technologies are currently being marketed to consumers so that this is going to create a lot of tension, particularly, I think with the practice community, and this is particularly -- so since evidence suggests a low level of genetic knowledge in consumers and low levels of skills to deal with that knowledge in providers. So I think genome research really has been particularly benefiting the basic scientists. I think the clinical investigators and the epidemiologists, I might say, added to that should really ready themselves to participate in this developing field. And I hope this course has helped to do that. So, any questions from mine, and then we'll just close it up. Yes? Microphone. [Female Speaker] I want to clarify something about access to the dbGaP database. We have some of our participants are involved in an ongoing GWA gene-environment study right now, and it's my understanding that the PI of the GWA study itself can specify what kinds of questions can be asked of the data. And so for example, in our situation, our consent form for collection of DNA samples in the first place was very specific about what kinds of analyses could be done. [Dr. Thomas Pearson] Yeah, I had only so much room on my slide. But thank you for the question, and maybe Teri would want to comment on this since she's been involved with all that. But the scenario you point out is, in fact, identified within the whole policy if you read it. And that is that some of the informed consent specifications about how the data could be not used, and that's what the person signed in terms of consent. And if some of those really basically suggested no other use or other use outside of this own study. I think that's the answer unless you want to go back to them and re-consent them, which obviously is a lot of work, as we all know. And so there is the ability to -- if there is a limitation on the evidence, an opportunity to cite what those limitations are and the reasons for those limitations, but I think you can't just limit the whole thing. [Dr. Teri Manolio] No, no, right. [Dr. Thomas Pearson] So it's not just -- you just can't say, "Oh, I don't want to play." [Dr. Teri Manolio] Yeah, or I don't want somebody to look at, you know, my favorite phenotype, whatever. Yeah, it's based on the consent. But we don't look at the consent forms, so there is an element of trust here. And obviously, if we saw something that looked a little bit suspicious, we'd ask someone. The limitations that we tend to see are used for a specific disease. So it tends to be, if this was a schizophrenia study, you only use it for schizophrenia. And the other one is often noncommercial use.  So if you are a for-profit user, there are some, usually about 10 percent, 5 percent of participants have, you know, issues with commercial use in drug companies and that, so those will be excluded then if you are a commercial user. But you still can get the rest of the data set. [Dr. Thomas Pearson] Well, this is potentially, obviously, an important paradigm in translation and certainly in our clinical translation of science awards, I think the idea was consistent with this is to open up to a much larger community of investigators because a lot of people, again, would go in, have their disease of interest, ask their question and then say, "I am done with it," leaving 99.9 percent of the data really unanalyzed.
History

Anticoagulation therapy has a long history. In 1884 John Berry Haycraft described a substance found in the saliva of leeches, Hirudo medicinalis, that had anticoagulant effects. He named the substance ‘Hirudine’ from the Latin name. The use of medicinal leeches can be dated back all the way to ancient Egypt.[2] In the early 20th century Jay McLean, L. Emmet Holt Jr. and William Henry Howell discovered the anticoagulant heparin, which they isolated from the liver (hepar).[3] Heparin remains one of the most effective anticoagulants and is still used today, although it has its disadvantages, such as requiring intravenous administration and having a variable dose-response curve due to substantial protein binding.[4] In the 1980s low molecular-weight heparin (LMWH) were developed. They are derived from heparin by enzymatic or chemical depolymerization and have better pharmacokinetic properties than heparin.[5] In 1955 the first clinical use of warfarin, a vitamin K antagonist, was reported. Warfarin was originally used as a rat poison in 1948 and thought to be unsafe for humans, but a suicide attempt suggested that it was relatively safe for humans. Vitamin K antagonists are the most commonly used oral anticoagulants today and warfarin was the 11th most prescribed drug in the United States in 1999[3] and is actually the most widely prescribed oral anticoagulant worldwide.[6] Warfarin has its disadvantages though, just like heparin, such as a narrow therapeutic index and multiple food and drug interactions and it requires routine anticoagulation monitoring and dose adjustment.[4][7] Since both heparin and warfarin have their downsides the search for alternative anticoagulants has been ongoing and DTIs are proving to be worthy competitors. The first DTI was actually hirudin, which became more easily available with genetic engineering. It is now available in a recombinant form as lepirudin (Refludan) and desirudin (Revasc, Iprivask). Development of other DTIs followed with the hirudin analog, bivalirudin, and then the small molecular DTIs.[4] However, such DTIs were also having side effects such as bleeding complications and liver toxicity, and their long-term effects were in doubt.[citation needed]
Mechanism of action
Blood clotting cascade

When a blood vessel ruptures or gets injured, factor VII comes into contact with tissue factors which starts a process called the blood coagulation cascade. Its purpose is to stop bleeding and repair tissue damage. When this process is too active due to various problems the risk of blood clots or embolisms increases. As the name indicates the cascade is a multi-step procedure where the main product thrombin is made by activating various proenzymes (mainly serine proteases) in each step of the cascade. Thrombin has multiple purposes, but mainly it converts soluble fibrinogen to an insoluble fibrin complex.[8] Furthermore, it activates factors V, VIII and XI, all by cleaving the sequences GlyGlyGlyValArg-GlyPro and PhePheSerAlaArg-GlyHis, selectively between Arginine (Arg) and Glycine (Gly).[9] These factors generate more thrombin. Thrombin also activates factor XIII that stabilizes the fibrin complex and therefore the clot and it stimulates platelets, which help with the coagulation. Given this broad action of thrombin it stands as a good drug target for anticoagulant drugs such as heparin, warfarin and DTIs and antiplatelet drugs like aspirin.[8][10][11]
Binding sites
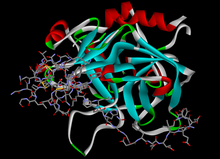
Thrombin is in the serine protease family. It has 3 binding domains in which thrombin-inhibition drugs bind to. Those proteases have a deep narrow gap as an active binding site that consists of two β-barrel subdomains that make up the surface gap which binds substrate peptides. The surface in the gap seems to have limiting access to molecules by steric hindrance, this binding site consists of 3 amino acids, Asp-102, His-57 and Ser-195.[9][12] Thrombin also has two exosites (1 and 2). Thrombin is a little different from other serine proteases as exosite 1 is anion-binding and binds to fibrin and other similar substrates while exosite 2 is a heparin-binding domain.[8][9]
DTIs inhibition

.
DTIs inhibit thrombin by two ways; bivalent DTIs block simultaneously the active site and exosite 1 and act as competitive inhibitors of fibrin,[13] while univalent DTIs block only the active site and can therefore both inhibit unbound and fibrin-bound thrombin. In contrast, heparin drugs bind in exosite 2 and form a bridge between thrombin and antithrombin, a natural anticoagulant substrate formed in the body, and strongly catalyzes its function. But heparin can also form a bridge between thrombin and fibrin which binds to exosite 1 which protects the thrombin from inhibiting function of heparin-antithrombin complex and increases thrombin's affinity to fibrin.[8] DTIs that bind to the anion-binding site have shown to inactivate thrombin without disconnecting thrombin from fibrin, which points to a separate binding site for fibrin.[12] DTIs aren't dependent to cofactors like antithrombin to inhibit thrombin so they can both inhibit free/soluble thrombin as well as fibrin bound thrombin unlike heparins.[10] The inhibition is either irreversible or reversible. Reversible inhibition is often linked to lesser risk of bleeding. Due to this action of DTIs they can both be used for prophylaxis as well as treatment for embolisms/clots.[8][10]
Active site's pockets

DTIs that fit in the active binding site have to fit in the hydrophobic pocket (S1) that contains aspartic acid residue at the bottom which recognizes the basic side chain. The S2 site has a loop around tryptophan which occludes a hydrophobic pocket that can recognize larger aliphatic residues. The S3 site is flat and the S4 site is hydrophobic, it has tryptophan lined by leucine and isoleucine.[9]

Nα-(2-naphthyl-sulphonyl-glycyl)-DL-p-amidinophenylalanyl-piperidine (NAPAP) binds thrombin in the S1, S2 and S4 pockets. The amidine group on NAPAP forms a bidentate salt bridge with Asp deep in the S1 pocket, the piperidine group takes the role of proline residue and binds in the S2 pocket, and the naphthyl rings of the molecule forms a hydrophobic interaction with Trp in the S4 pocket. Pharmaceutical companies have used the structural knowledge of NAPAP to develop DTIs. Dabigatran, like NAPAP binds to S1, S2 and S4 pockets. Benzamidine group on the dabigatran structure binds deep in the S1 pocket, the methylbenzimidazole fits nicely in the hydrophobic S2 pocket and the Ile and Leu at the bottom of the S4 pocket binds to the aromatic group of dabigatran.[9]
Drug development
Hirudin derivatives
Hirudin derivatives are all bivalent DTIs, they block both the active site and exosite 1 in an irreversible 1:1 stoichiometric complex.[4] The active site is the binding site for the globular amino-terminal domain and exosite 1 is the binding site for the acidic carboxy-terminal domain of hirudin.[14] Native hirudin, a 65-amino-acid polypeptide, is produced in the parapharyngeal glands of medicinal leeches.[15] Hirudins today are produced by recombinant biotechnology using yeast. These recombinant hirudins lack a sulfate group at Tyr-63 and are therefore called desulfatohirudins. They have a 10-fold lower binding affinity to thrombin compared to native hirudin, but remain a highly specific inhibitor of thrombin and have an inhibition constant for thrombin in the picomolar range.[14][15] Renal clearance and degradation account for the most part for the systemic clearance of desulfatohirudins and there is accumulation of the drug in patients with chronic kidney disease. These drugs should not be used in patients with impaired renal function, since there is no specific antidote available to reverse the effects.[14] Hirudins are given parenterally, usually by intravenous injection. 80% of hirudin is distributed in the extravascular compartment and only 20% is found in the plasma. The most common desulfatohirudins today are lepirudin and desirudin.[15]
Hirudin
In a meta-analysis of 11 randomized trials involving hirudin and other DTIs versus heparin in the treatment of acute coronary syndrome (ACS) it was found that hirudin has a significantly higher incidence of bleeding compared with heparin. Hirudin is therefore not recommended for treatment of ACS and currently it has no clinical indications.[4]
Lepirudin

Lepirudin is approved for the treatment of heparin-induced thrombocytopenia (HIT) in the USA, Canada, Europe and Australia. HIT is a very serious adverse event related to heparin and occurs with both unfractionated heparin and LMWH, although to a lesser extent with the latter. It is an immune-mediated, prothrombotic complication which results from a platelet-activating immune response triggered by the interaction of heparin with platelet factor 4 (PF4).[16] The PF4-heparin complex can activate platelets and may cause venous and arterial thrombosis.[8] When lepirudin binds to thrombin it hinders its prothrombic activity.[16] Three prospective studies, called the Heparin-Associated-Thrombocytopenia (HAT) 1,2, and 3, were performed that compared lepirudin with historical controls in the treatment of HIT. All three studies showed that the risk of new thrombosis was decreased with the use of lepirudin, but the risk for major bleeding was increased.[15] The higher incidence of major bleeding is thought to be the result of an approved dosing regimen that was too high, consequently the recommended dose was halved from the initial dose.[4] As of May 2012 Bayer HealthCare, the only manufacturer of lepirudin injections, discontinued its production. They expect supplies from wholesalers to be depleted by mid-2013.[17]
Desirudin
Desirudin is approved for treatment of venous thromboembolism (VTE) in Europe and multiple phase III trials are presently ongoing in the USA.[4] Two studies comparing desirudin with enoxaparin (a LMWH) or unfractionated heparin have been performed. In both studies desirudin was considered to be superior in preventing VTE. Desirudin also reduced the rate of proximal deep vein thrombosis. Bleeding rates were similar with desirudin and heparin.[4][8]
Bivalirudin

Bivalirudin, a 20 amino acid polypeptide, is a synthetic analog of hirudin. Like the hirudins it is also a bivalent DTI. It has an amino-terminal D-Phe-Pro-Arg-Pro domain that is linked via four Gly residues to a dodecapeptide analog of the carboxy-terminal of hirudin. The amino-terminal domain binds to the active site and the carboxy-terminal domain binds to exosite 1 on thrombin. Different from the hirudins, once bound thrombin cleaves the Arg-Pro bond at the amino-terminal of bivalirudin and as a result restores the functions to the active site of the enzyme. Even though the carboxy-terminal domain of bivalirudin is still bound to exosite 1 on thrombin, the affinity of the bond is decreased after the amino-terminal is released. This allows substrates to substrates to compete with cleaved bivalirudin for access to exosite 1 on thrombin.[14] The use of bivalirudin has mostly been studied in the setting of acute coronary syndrome. A few studies indicate that bivalirudin is non-inferior compared to heparin and that bivalirudin is associated with a lower rate of bleeding.[4] Unlike the hirudins, bivalirudin is only partially (about 20%) excreted by the kidneys, other sites such as hepatic metabolism and proteolysis also contribute to its metabolism, making it safer to use in patients with renal impairment; however, dose adjustments are needed in severe renal impairment.[8][16]
Small molecular direct thrombin inhibitors
Small molecular direct thrombin inhibitors (smDTIs) are non-peptide small molecules that specifically and reversibly inhibit both free and clot-bound thrombin by binding to the active site of the thrombin molecule. They prevent VTE in patients undergoing hip- and knee replacement surgery.[10] The advantages of this type of DTIs are that they do not need monitoring, have a wide therapeutic index and the possibility of oral administration route. They are theoretically more convenient than both vitamin K antagonist and LMWH. Researches will, however, have to show the indication of the use and their safety.[18]
The smDTIs where derived using a peptidomimetic design with either P1 residue from arginine itself (e.g. argatroban) or arginine-like substrates such as benzamidine (e.g. NAPAP).[9]
Argatroban

Argatroban is a small univalent DTI formed from P1 residue from arginine. It binds to the active site on thrombin.[10] The X-ray crystal structure shows that the piperidine ring binds in the S2 pocket and the guanidine group binds with hydrogen bonds with Asp189 into the S1 pocket. It’s given as an intravenous bolus because the highly basic guanidine with pKa 13 prevents it to be absorbed from the gastrointestinal tract.[19] The plasma half-life is approximately 45 minutes. As argatroban is metabolized via hepatic pathway and is mainly excreted through the biliary system, dose adjustments are necessary in patients with hepatic impairment but not renal damage. Argatroban has been approved in the USA since 2000 for the treatment of thrombosis in patients with HIT and 2002 for anticoagulation in patients with a history of HIT or are at risk of HIT undergoing percutaneous coronary interventions (PCI).[10][19] It was first introduced in Japan in 1990 for treatment of peripheral vascular disorders.[19]
Ximelagatran
The publication of the NAPAP-fIIa crystal structure triggered many researches on thrombin inhibitors. NAPAP is an active site thrombin inhibitor. It fills the S3 and S2 pockets with its naphthalene and piperidine groups. AstraZeneca used the information to develop melagatran. The compound was poorly orally available, but after renovation they got a double prodrug which was the first oral DTI in clinical trials, ximelagatran.[9] Ximelagatran was on the European market for approximately 20 months when it was suspended. Studies showed that treatment for over 35 days was linked with the risk of hepatic toxicity.[18] It was never approved by the FDA.[20]

Dabigatran etexilate
Researchers at Boehringer Ingelheim also used the publicized information about the NAPAP-fIIa crystal structure, starting with the NAPAP structure that led to the discovery of dabigatran,[9] which is a very polar compound and therefore not orally active. By masking the amidinium moiety as a carbamate-ester and turning the carboxylate into an ester they were able to make a prodrug called dabigatran etexilate,[21] a highly lipophilic, gastrointestinally absorbed and orally bioavailable double prodrug such as ximelagatran, with the plasma half-life of approximately 12 hours.[9] Dabigatran etexilate is rapidly absorbed, it lacks interaction with cytochrome P450 enzymes and with other food and drugs, there is no need for routine monitoring and it has a broad therapeutic index and a fixed-dose administration, which is excellent safety compared with warfarin.[4] Unlike ximelagatran, a long-term treatment of dabigatran etexilate has not been linked with hepatic toxicity, seeing as how the drug is predominantly eliminated (>80%) by the kidneys. Dabigatran etexilate was approved in Canada and Europe in 2008 for the prevention of VTE in patients undergoing hip- and knee surgery. In October 2010 the US FDA approved dabigatran etexilate for the prevention of stroke in patients with atrial fibrillation (AF).[6][10] Many pharmaceutical companies have attempted to develop orally bioavailable DTI drugs but dabigatran etexilate is the only one to reach the market.[9]
In a 2012 meta-analysis dabigatran was associated with increased risk of myocardial infarction (MI) or ACS when tested against different controls in a broad spectrum of patients.[22]

Table 1: Summary of characteristics of DTIs
| Bivalent/ Univalent[4] | Route of administration[10] | Metabolism[10] | Binding to active site and/or exosite 1[4] | Indications | Limitations | Advantages | |
| Native Hirudin | B | (Parenteral) | Has no indications | ||||
| Lepirudin | B | Parenteral (iv/sc) | Renal | Irreversible | Prevention of further thrombosis in patients with HIT[16] | Narrow TI, potential increased bleedings, antihirudid antibodies are formed in 40% of patients, need for weight-based dosing[10] | |
| Desirudin | B | Parenteral (iv/sc) | Renal | Irreversible | Europe: treatment of VTE[4] USA: Prevention of DVT in patients undergoing hip replacement surgery[23] | Less need for weight-based doses and routine monitoring compared to lepirudin because of sc administration[10] | |
| Bivalirudin | B | Parenteral (iv) | Proteolytic cleavage, hepatic, 20% renal | Reversible | Prevention of acute ischemic complications in patients with unstable angina and with or at risk of HIT undergoing PTCA or PCI[24] | Dose adjustments are needed in severe renal impairment[16] | Decreased bleeding risk due to reversible binding,[4] improved safety profile compared with r-hirudins, fast onset of action[10] |
| Argatroban | U | Parenteral (iv) | Hepatical, mostly biliary | Reversible | Prevention and treatment of thrombosis in patients with HIT[10] | No bolus dose needed[10] | |
| Ximelagatran | U | Oral | Hepatic | Reversible | Europe: Prevention of VTE[10]
USA: FDA never gave approval[20] |
Long-term therapy (›35 days) is associated to hepatotoxicity – taken off market in Europe[18] | |
| Dabigatran etexilate | U | Oral | Primarily renal, remainder is conjugated with glucuronic acid in liver | Reversible | Prevention of stroke and embolism in patients with AF[25] | Rapid onset of action, lack of interaction with CYP450, food or drugs, broad TI, fixed dose administration and good safety profile, not associated with hepatotoxicity for long-term use[10] |
iv: intravenous, sc: subcutaneous, HIT: heparin-induced thrombocytopenia, VTE: Venous thromboembolism, DVT: Deep vein thrombosis, PTCA: Percutaneous transluminal coronary angioplasty, PCI: percutaneous coronary intervention, FDA: Food and Drug Administration, AF: Atrial fibrillation, TI: Therapeutic index
Status 2014
In 2014 dabigatran remains the only approved oral DTI[9] and is therefore the only DTI alternative to the vitamin K antagonists. There are, however, some novel oral anticoagulant drugs that are currently in early and advanced stages of clinical development. Most of those drugs are in the class of direct factor Xa inhibitors, but there is one DTI called AZD0837,[26] which is a follow-up compound of ximelgatran that is being developed by AstraZeneca. It is the prodrug of a potent, competitive, reversible inhibitor of free and fibrin-bound thrombin called ARH0637.[18] The development of AZD 0837 is discontinued. Due to a limitation identified in long-term stability of the extended-release AZD0837 drug product, a follow-up study from ASSURE on stroke prevention in patients with non-valvular atrial fibrillation, was prematurely closed in 2010 after 2 years. There was also a numerically higher mortality against warfarin.[27][28][29] In a Phase 2 trial for AF the mean serum creatinine concentration increased by about 10% from baseline in patients treated with AZD0837, which returned to baseline after cessation of therapy.[30] Development of other oral DTIs, such as Sofigatran from Mitsubishi Tanabe Pharma has been discontinued.[26] Another strategy for developing oral anticoagulant drugs is that of dual thrombin and fXa inhibitors that some pharmaceutical companies, including Boehringer Ingelheim, have reported on. These compounds show favorable anticoagulant activity in vitro.[9]
See also
References
- ^ Mehta, AY; Jin, Y; Desai, UR (Jan 2014). "An update on recent patents on thrombin inhibitors (2010 - 2013)". Expert Opinion on Therapeutic Patents. 24 (1): 47–67. doi:10.1517/13543776.2014.845169. PMID 24099091. S2CID 24817396.
- ^ Whitacker, I.S.; Rao, J.; Izadi, D.; Butler, P.E. (2004). "Historical Article: Hirudo medicinalis: ancient origins of, and trends in the use of medicinal leeches throughout history". British Journal of Oral and Maxillofacial Surgery. 42 (2): 133–137. doi:10.1016/S0266-4356(03)00242-0. PMID 15013545.
- ^ a b Shapiro, Sandor S. (2003). "Treating Thrombosis in the 21st Century". New England Journal of Medicine. 349 (18): 1762–1764. doi:10.1056/NEJMe038152. PMID 14585945.
- ^ a b c d e f g h i j k l m n O’Brien, P. Joshua; Mureebe, Leila (2012). "Direct Thrombin Inhibitors". Journal of Cardiovascular Pharmacology and Therapeutics. 17 (1): 5–11. doi:10.1177/1074248410395941. PMID 21335484. S2CID 6771526.
- ^ Hirsh, Jack; Raschke, Robert (2004). "Heparin and Low-Molecular-Weight Heparin The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy". Chest. 126 (3_suppl): 188S–203S. doi:10.1378/chest.126.3_suppl.188s. PMID 15383472.
- ^ a b Thethi, Indermohan; Lewis, Bruce; Fareed, Jawed (1 January 2012). "Oral Factor Xa and Direct Thrombin Inhibitors". Journal of Burn Care & Research. 33 (4): 453–461. doi:10.1097/BCR.0b013e318248bc4c. PMID 22269826. S2CID 3665578.
- ^ Kendoff, D. (30 December 2011). "Oral Thromboprophylaxis Following Total Hip or Knee Replacement: Review and Multicentre Experience with Dabigatran Etexilate". The Open Orthopaedics Journal. 5 (1): 395–399. doi:10.2174/1874325001105010395. PMC 3263520. PMID 22276081.
- ^ a b c d e f g h Di Nisio, Marcello J.; Middeldorp, Saskia; Büller, Harry R. (2005). "Direct Thrombin Inhibitors". New England Journal of Medicine. 353 (10): 1028–1040. doi:10.1056/NEJMra044440. PMID 16148288.
- ^ a b c d e f g h i j k l Nar, Herbert (2012). "The role of structural information in the discovery of direct thrombin and factor Xa inhibitors". Trends in Pharmacological Sciences. 33 (5): 279–288. doi:10.1016/j.tips.2012.03.004. PMID 22503439.
- ^ a b c d e f g h i j k l m n o p Lee, Catherine J.; Ansell, Jack E. (2011). "Direct Thrombin Inhibitors". British Journal of Clinical Pharmacology. 72 (4): 581–592. doi:10.1111/j.1365-2125.2011.03916.x. PMC 3195735. PMID 21241354.
- ^ Patrono, C (May 5, 1994). "Aspirin as an antiplatelet drug". New England Journal of Medicine. 330 (18): 1287–1294. doi:10.1056/NEJM199405053301808. PMID 8145785. WOS:A1994NJ51200008.
- ^ a b Lefkovits, J.; Topol, E.J (1994). "Direct thrombin inhibitors in cardiovascular medicine". Circulation. 90 (3): 1522–1536. doi:10.1161/01.CIR.90.3.1522. PMID 8087958.
- ^ Thomas, edited by Simon Redwood, Nick Curzen, Martyn R. (2010). Oxford textbook of interventional cardiology (1. publ. ed.). Oxford: Oxford University Press. ISBN 978-0-19-956908-3.
{{cite book}}:|first=has generic name (help)CS1 maint: multiple names: authors list (link) - ^ a b c d Weitz, Jeffery I.; Crowther, Mark (2002). "Direct Thrombin Inhibitors". Thrombosis Research. 106 (3): 275–284. doi:10.1016/S0049-3848(02)00093-2. PMID 12356489.
- ^ a b c d Greinacher, Andreas; Warkentin, Theadore E. (2008). "The direct thrombin inhibitor hirudin". Thrombosis and Haemostasis. 99 (5): 819–829. doi:10.1160/TH07-11-0693. PMID 18449411.
- ^ a b c d e Sakr, Yasser (2011). "Heparin-induced thrombocytopenia in the ICU: an overview". Critical Care. 15 (2): 211. doi:10.1186/cc9993. PMC 3219407. PMID 21457505.
- ^ "Lepirudin Injection". American Society of Health-System Pharmacists. Retrieved 18 September 2012.
- ^ a b c d Squizzato, A; Dentali F.; Steidi L.; Ageno W. (2009). "New direct thrombin inhibitors". Intern Emerg Med. 4 (6): 479–484. doi:10.1007/s11739-009-0314-8. PMID 19756950. S2CID 25332427.
- ^ a b c Kikelj, Danijel. (2004). "Peptidomimetic Thrombin Inhibitors". Pathophysiology of Haemostasis and Thrombosis. 33 (5–6): 487–491. doi:10.1159/000083850. PMID 15692265.
- ^ a b heartwire. "FDA opts not to approve ximelagatran". Retrieved 19 September 2012.
- ^ Hauel, Norbert H.; Nar, Herbert; Priepke, Henning; Ries, Uwe; Stassen, Jean-Marie; Wienen, Wolfgang (2002). "Structure-Based Design of Novel Potent Nonpeptide Thrombin Inhibitors". Journal of Medicinal Chemistry. 45 (9): 1757–1766. doi:10.1021/jm0109513. PMID 11960487.
- ^ Uchino, K.; Hernandez, A. V. (9 January 2012). "Dabigatran Association With Higher Risk of Acute Coronary Events: Meta-analysis of Noninferiority Randomized Controlled Trials". Archives of Internal Medicine. 172 (5): 397–402. doi:10.1001/archinternmed.2011.1666. PMID 22231617.
- ^ "Iprivask 15 mg" (PDF). Retrieved 18 September 2012.
- ^ "Angiomax Injection" (PDF). Food and Drug Administration. Retrieved 18 September 2012.
- ^ "FDA approves Pradaxa to prevent stroke in people with atrial fibrillation". Food and Drug Administration. Retrieved 18 September 2012.
- ^ a b Ahrens, Ingo; Karlheinz Peter; Gregory Y.H. Lip; Christoph Bode (2012). "Development and Clinical Applications of Novel Oral Anticoagulants. Part II. Drugs Under Clinical Investigation". Discovery Medicine. 13 (73): 445–450. PMID 22742650.
- ^ "AZD0837". Astrazenecaclinicaltrials.com. Retrieved 2012-10-16.
- ^ AstraZeneca Long-term treatment with the oral direct thrombin inhibitor AZD0837, compared to Vitamin-K antagonists, as stroke prevention in patients with non-valvular atrial fibrillation and one or more risk factors for stroke and systemic embolic events. A 5-year follow-up study study code D1250C0004221 January 2010 Trial D1250C00042 Archived November 10, 2013, at the Wayback Machine
- ^ Eikelboom JW, Weitz JI (2010). "Update on Antithrombotic Therapy: New Anticoagulants". Circulation. 121 (13): 1523–32. doi:10.1161/CIRCULATIONAHA.109.853119. PMID 20368532.
- ^ Lip GY, Rasmussen LH, Olsson SB, Jensen EC, Persson AL, Eriksson U, Wåhlander KF (December 2009). "Oral direct thrombin inhibitor AZD0837 for the prevention of stroke and systemic embolism in patients with non-valvular atrial fibrillation: a randomized dose-guiding, safety, and tolerability study of four doses of AZD0837 vs. vitamin K antagonists". Eur. Heart J. 30 (23): 2897–907. doi:10.1093/eurheartj/ehp318. PMC 2785945. PMID 19690349.
