| Platysma muscle | |
|---|---|
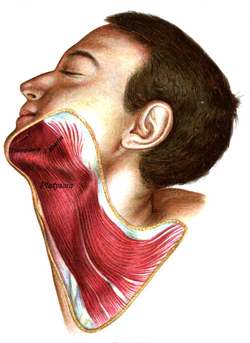 The platysma is visible, with skin removed. | |
 The muscles of the face, platysma visible at bottom right. | |
| Details | |
| Origin | subcutaneous tissue of infraclavicular and supraclavicular regions |
| Insertion | base of mandible; skin of cheek and lower lip; angle of mouth; orbicularis oris |
| Artery | branches of the submental artery and suprascapular artery |
| Nerve | cervical branch of the facial nerve |
| Actions | draws the corners of the mouth inferiorly and widens it (as in expressions of sadness and fright). Also draws the skin of the neck superiorly when teeth are clenched |
| Antagonist | masseter muscle, temporalis muscle |
| Identifiers | |
| Latin | platysma |
| TA98 | A04.2.01.001 |
| TA2 | 2147 |
| FMA | 45738 |
| Anatomical terms of muscle | |
The platysma muscle is a superficial muscle of the human neck that overlaps the sternocleidomastoid. It covers the anterior surface of the neck superficially. When it contracts, it produces a slight wrinkling of the neck, and a "bowstring" effect on either side of the neck.
YouTube Encyclopedic
-
1/5Views:101 2457 0268 3103 5522 934
-
Platysma muscle - Origin, Insertion, Innervation & Function - Human Anatomy | Kenhub
-
Platysma Muscle - Massage Anatomy
-
Platysma muscle
-
Two Minutes of Anatomy: Platysma Muscle
-
Platysma | Structure & Functions
Transcription
Structure
The platysma muscle is a broad sheet of muscle arising from the fascia covering the upper parts of the pectoralis major muscle and deltoid muscle. Its fibers cross the clavicle, and proceed obliquely upward and medially along the side of the neck. This leaves the inferior part of the neck in the midline deficient of significant muscle cover.[1]
Fibres at the front of the muscle from the left and right sides intermingle together below and behind the mandibular symphysis, the junction where the two lateral halves of the mandible are fused at an early period of life (although not a true symphysis). Fibres at the back of the muscle cross the mandible, some being inserted into the bone below the oblique line, others into the skin and subcutaneous tissue of the lower part of the face. Many of these fibers blend with the muscles about the angle and lower part of the mouth.[1]
Sometimes fibers can be traced to the zygomaticus major muscle, or to the margin of the orbicularis oris muscle. Beneath the platysma, the external jugular vein descends from the angle of the mandible to the clavicle.[2]
Nerve supply
The platysma muscle is supplied by the cervical branch of the facial nerve.[1]
Blood supply
The platysma muscle is supplied by branches of the submental artery and suprascapular artery.
Relations
The platysma muscle lies just deep to the subcutaneous fascia and fat.[1][3] It covers many structures found deeper in the neck, such as the external carotid artery, the external jugular vein,[4] the parotid gland,[4] the lesser occipital nerve,[4] the great auricular nerve,[4] and the marginal mandibular branch of the facial nerve.[5]
Variation
Variations occur in the extension over the face and over the clavicle and shoulder. The platysma muscle may be absent or interdigitate with the muscle of the opposite side in front of the neck; attachment to clavicle, mastoid process or occipital bone occurs. A more or less independent fasciculus, the occipitalis minor muscle, may extend from the fascia over the trapezius muscle to fascia over the insertion of the sternocleidomastoid muscle.
Function
Wrinkling
When the entire platysma muscle is in action, it produces a slight wrinkling of the surface of the skin of the neck in an oblique direction (at an angle to the midline). It creates a distinctive "bowstring" effect on either side of the neck, where fibres move away from the midline.[3]
Jaw and lip movement
The anterior portion of the platysma muscle, the thickest part of the muscle, depresses the lower jaw. It also draws down the lower lip and angle of the mouth in a frown. However, the platysma muscle plays only a minor role in depressing the lower lip, which is primarily performed by the depressor anguli oris muscle and the depressor labii inferioris muscle.
Clinical significance
In a similar fashion to other muscles, the platysma muscle is vulnerable to tears, strains and muscle atrophy, among many other possible conditions.
Injury
The platysma muscle is vulnerable to neck injuries that may penetrate it, as it is both superficial and thin.[6] Penetrating trauma in the neck injuries can be defined as any that completely penetrate the platysma muscle, making it an important landmark.[6] Computed tomography angiography may be used to visualise arteries and veins, such as for complex injuries from gunshot wounds or stab wounds, and is useful to image any damage to the muscle.[6][7] This minimises the number of exploratory surgeries that need to be performed, thus improving the handling of the condition.[7]
Neck surgery
When neck surgery is performed, the platysma muscle usually needs to be cut through to access deeper structures.[1][5] Fibres need to be sutured together accurately to prevent abnormal scar retraction, which may look unsightly.[1]
Plastic surgery
Wrinkly skin of neck caused by decrease in muscle tone leading to thinning and shortening of muscle is the secondary complication of facial nerve palsy and can be associated with the normal aging process. Neck bands in the area above the platysma muscle become most noticeable with age.[3] These may be aggravated by weightlifting or facelift procedures. This may be known as platysma dyskinesia or "turkey neck".
Conservative management may be used. Alternatively, interventions include botulinum toxin injection and platysmaplasty. Platysmaplasty is a surgery in this area, that can be open or closed; in the latter a specialised instrument called a plastymotome is used that allows the surgery to be done without incisions.[8] It takes approximately 2 weeks for the symptoms to be reduced.[9]
Adipose tissue is found above the platysma muscle, so liposuction of the neck may be performed fairly easily without the need to pierce it.[10] It is also important to not damage the platysma muscle to prevent bleeding.[10]
Images
-
Platysma is visible at bottom, in neck
References
![]() This article incorporates text in the public domain from page 387 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 387 of the 20th edition of Gray's Anatomy (1918)
- ^ a b c d e f Eibling, David E. (2008). "78 - Neck Dissection". Operative Otolaryngology: Head and Neck Surgery. Vol. 1 (2nd ed.). Philadelphia: Saunders. pp. 679–708. doi:10.1016/B978-1-4160-2445-3.50082-0. ISBN 978-1-4377-2083-9. OCLC 825780332.
- ^ Kim, Se-Hoon; Chang, Ung-Kyu; Kim, Daniel H.; Bilsky, Mark H. (2006-01-01), Kim, Daniel H.; Chang, Ung-Kyu; Kim, Se-Hoon; Bilsky, Mark H. (eds.), "Chapter 19 - Management of Upper Cervical Spine Tumors", Tumors of the Spine, Philadelphia: W.B. Saunders, pp. 378–394, ISBN 978-1-4160-3367-7, retrieved 2021-01-06
- ^ a b c Posnick, Jeffrey C. (2014). "40 - Aesthetic Alteration of the Soft Tissues of the Neck and Lower Face: Evaluation and Surgery". Orthognathic Surgery: Principles & Practice. St. Louis: Saunders. pp. 1746–1783. doi:10.1016/B978-1-4557-2698-1.00040-X. ISBN 978-1-4557-5027-6. OCLC 860861780.
- ^ a b c d Kim, Se-Hoon; Chang, Ung-Kyu; Kim, Daniel H.; Bilsky, Mark H. (2008). "19 - Management of Upper Cervical Spine Tumors". Tumors of the Spine. Philadelphia: Saunders. pp. 378–394. doi:10.1016/B978-1-4160-3367-7.10019-7. ISBN 978-1-4377-2164-5. OCLC 489078564.
- ^ a b Wolfe, Michael J.; Wilson, Keith (2007). "21 - Head and Neck Cancer". Essentials of Surgical Oncology: Surgical Foundations. Philadelphia: Mosby. pp. 329–357. doi:10.1016/B978-0-8151-4385-7.50027-8. ISBN 978-0-8151-4385-7. OCLC 608607674.
- ^ a b c Cothren, C. Clay; Moore, Ernest E. (2009). "19 - Penetrating Neck Trauma". Abernathy's Surgical Secrets (6th ed.). Philadelphia: Mosby. pp. 110–113. doi:10.1016/B978-0-323-05711-0.00019-7. ISBN 978-0-323-07475-9. OCLC 460933202.
- ^ a b Bell, RB; Osborn, T; Dierks, EJ; Potter, BE; Long, WB (2007). "Management of penetrating neck injuries: a new paradigm for civilian trauma". J. Oral Maxillofac. Surg. 65 (4): 691–705. doi:10.1016/j.joms.2006.04.044. PMID 17368366.
- ^ Labb??n a similar fashion to other muscles, the platysma is vulnerable to tears, strains and muscle atrophy among many other possible conditions. The platysma is vulnerable to neck injuries that may penetrate it. A type of medical imaging called CTA (computed tomography angiography), used to visualise arterial and venous vessels, is useful to minimise the number of neck explorations, thus improving the handling of the condition.[3] Another area of importance of the platysma lies in plastic surgery. Neck bands in the area become most noticeable with age, aggravated by weightlifting or facelift. If it doesn't heal with time, there are many options to correct this: Botox/Dysport/Xeomin and platysmaplasty. Platysmaplasty is a surgery in this area, that can be open or closed, in the latter a specialised instrument called plastymotome that allow the surgery to be done without incisions. It takes approximately 2 weeks for the symptoms to be reduced.[4], Daniel; Franco, R G.; Nicolas, J (May 2006). "Platysma Suspension and Platysmaplasty during Neck Lift: Anatomical Study and Analysis of 30 Cases". Plastic and Reconstructive Surgery. 117 (6): 2001–2007. doi:10.1097/01.prs.0000218972.75144.9c. ISSN 0032-1052. PMID 16651976. S2CID 26104853.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: numeric names: authors list (link) - ^ Daher, JC (2011). "Closed platysmotomy: a new procedure for the treatment of platysma bands without skin dissection". Aesthetic Plast Surg. 35 (5): 866–77. doi:10.1007/s00266-011-9782-0. PMC 3192284. PMID 21847680.
- ^ a b Alam, Murad; White, Lucile E. (2008). "1 - Anatomy in Dermatologic Surgery". Complications in Dermatologic Surgery. Philadelphia: Mosby. pp. 1–18. doi:10.1016/B978-0-323-04546-9.10001-9. ISBN 978-0-323-04546-9. OCLC 811786617.
- Books
- Susan Standring; Neil R. Borley; et al., eds. (2008). Gray's anatomy : the anatomical basis of clinical practice (40th ed.). London: Churchill Livingstone. ISBN 978-0-8089-2371-8.

