 | |
| Clinical data | |
|---|---|
| Trade names | Acodeen, Codesin, Pertix, Sinecod, Sinecoden, Sinecodix |
| AHFS/Drugs.com | International Drug Names |
| ATC code | |
| Pharmacokinetic data | |
| Protein binding | 98% |
| Elimination half-life | 6 hours |
| Excretion | 90% renal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.038.172 |
| Chemical and physical data | |
| Formula | C18H29NO3 |
| Molar mass | 307.434 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Butamirate (or brospamin, trade names Acodeen, Codesin, Pertix, Sinecod, Sinecoden, Sinecodix) is a cough suppressant.[1] It has been marketed in Europe and Mexico, but not in the United States.[2]
It is sold in the form of lozenges, syrup, tablets, dragées, or pastilles as the citrate salt. Adverse effects can include nausea, diarrhea, vertigo, and exanthema.[2]
YouTube Encyclopedic
-
1/3Views:214 6671 4975 863
-
Pharmacokinetics for Students: Absorption, Distribution, Metabolism, and Elimination -Lect 1
-
The Generics Pharmacy Philippines Guaifenesin Expectorant Cough Medicine BebotsOnly
-
Pharma Tube - 76 - Respiratory - 3 - Cough [HD]
Transcription
So let's jump right in to pharmacokinetics. So the first thing we want to do is be able to answer the question, what is pharmacokinetics and cover some basic definitions. And the easiest way to understand pharmacokinetics is to differentiate it from pharmacodynamics. So when you look at this word, pharmacokinetics, what is the first thing that you think of? Well, you should say pharmaco that means drug and kinetics, you should be thinking motion. And this is to differentiate pharmacokinetics from pharmacodynamics. Now, pharmaco again means drug. Dynamics comes from this word dynamus which really means power. So when I think of pharmacokinetics, I'm thinking of a drug and I'm thinking of that drug moving through our body. So what happens as a drug moves through our body? Well the concentration changes and that's really what pharmacokinetics is looking at. PK, pharmacokinetics, is really answering the question of how does the drug concentration change as it moves through the different compartments of your body. That is pharmacokinetics my friend. This is different than pharmacodynamics. We're dealing with power. When you think of somebody who is powerful, what can they do? They can exert their power and change other people right? So the same idea goes with pharmacodynamics. It's how does the drug exert its effects on your body, how powerful is this drug, how potent is it? So we deal with things like potency. Potency is a component of pharmacodynamics but by enlarge, the big thing we're looking at with pharmacodynamics is drug receptor interactions. Now we also look at efficacy of the effects of the drug. Potency refers to the you know how much of the drug is required to get a certain effect but we'll cover all of that later. Today we're really focused on pharmacokinetics. Now before we move any further, I want to explain how many books define this and how it can be confusing. So a lot of books define pharmacokinetics as what your body does to the drug and conversely, they define pharmacodynamics as what the drug does to your body. I always mix these things two up and I have to think about it and I always return back to my bread and butter right here. Pharmacokinetics, oh that has to do with motion, that has to do with the drug concentration changing as it's moving through my body. Pharmacodynamics, I think power. How does the drug exert its effects, drug receptor interactions, potency, efficacy - all that jack. So when I think of kinetics, where is it moving? Well drugs need to enter our body and so, half of pharmacokinetics is dealing with drugs entering our body and the other half of it is dealing with drugs leaving our body. They need to enter. They need to leave. So, what are the components of pharmacokinetics? So instead of writing enter and leave, I wrote in vs. out. So there are 2 components of drugs coming into our body. Those two components are represented with absorption (A) and distribution (D). I'm just going to write an A here and a D there. So what is absorption? Well, here's a book definition. Absorption is the process of a substance entering the blood circulation. It's okay. How can we make this definition a little better? Well, instead of saying our blood circulation, let's say it's the process of a substance entering the systemic circulation. and the reason I like to say systemic is because absorption is everything that happens before this drug enters our systemic circulation. So maybe I'll even add a little before right here. And if you think about, you take a drug orally, it goes through your intestines. It needs to go through your portal circulation before it gets to your liver and then it finally gets into your IVC then it's in our systemic circulation. So everything before that is what we call absorption. Now, to differentiate that from distribution, after it's in our systemic circulation, that drug can now be distributed to the rest of the body. So what is distribution? Well, here's a definition that is nothing special. The dispersion of well, maybe a substance throughout fluids and tissues of the body. It makes sense. You know you don't need a definition for distribution. It's going from one place to another. So those are the 2 ins. What are the 2 outs? How do drugs leave our body? Well one of them is metabolism and the other is elimination (E). And so, I'm going to write those right here. A, D, M, E. This is a little acronym that is commonly used to define the 4 components of pharmacokinetics. Absorption, Distribution, Metabolism, Elimination. So, what is metabolism? So, here's a definition that I do like. Metabolism is the irreversible transformation of parent compounds into daughter compounds. So what do we mean? Well, let's say I start with Drug A. I transform Drug A - it's the parent - into a very structurally similar daughter compound that is Drug B. Now, this doesn't mean that I am actually breaking down the drug. In pharmacology, it's actually the opposite. Many times we don't actually break down the drug but we actually add something to it and we add 1 or 2 molecules and the reason we do that is to make it more polar. And so, the reason we make it more polar is to help us eliminate it. Now before we move on to the next step, what are we doing here? We're taking a biologically active molecule and we're transforming it. So, a common name for metabolism is biotransformation. And so, what is doing this biotransformation? This is being done by enzymes. And the reason we do it again is to make it more polar to get it ready for elimination. Now this isn't the only reason that this happens but it's the big one and right now, we're focused on the big picture. So, elimination. What is elimination? Elimination is the removal of substances from the body. Now, the definition is not bad but the word itself is something I don't like. I don't like calling this elimination. Here's why. Look at what we did to Drug A right here. We started with Drug A, we biotransformed it and now we have Drug B. So in essence, what have we done with Drug A? Well, we've eliminated it right? And we no longer have Drug A. It goes bye-bye and now, we have Drug B. So metabolism is in a sense elimination and instead of calling this elimination, let's call this excretion. Now a lot of books mess this up and confuse these two. You might see this in your book written as elimination. Don't let yourself get confused but make sure you differentiate elimination from excretion. So it's important to know these definitions but it's even more important to know where these things are occurring in the body. So, let's do that. So where are you excreting or how do you excrete most of you know foreign substances in your body, most drugs? And most of the time, this is happening in your renal circulation. Let's write renal, let's write this is happening in your kidney. So when you see a kidney, a renal in some sort of exam question dealing with pharmacology, you can be thinking about excretion. Whereas metabolism, where is most biotransformation occurring? Let me ask you a question. Do you guys remember unconjugated bilirubin which came from red blood cells? Well, what was the problem with unconjugated bilirubin right? It needed to be conjugated and become direct bilirubin so that we can excrete it. Now where did that occur? Well that occurred in the liver. The same place where metabolism is occurring here. This is occurring in the liver. When you think liver, you should be thinking metabolism. Now, I'm going to note. We don't always do this to make it more polar. In some cases, we actually metabolize drugs to activate them and we've seen this in the body too. Where else have you seen the liver activate certain endogenous substances? Well, what about zymogens right? How did those get activated? Well those were metabolized and maybe not necessarily in the liver but you know we go from trypsinogen to trypsin, pepsinogen to pepsin. So metabolism, the definition is irreversible transformation of a parent compound to a daughter compound but when we deal with pharmacology, our goal is to do that to eliminate it. Distribution - so distribution was we're dealing with things going from one place to another after they're in our systemic circulation. So, where is this occurring? Well, what I want you to attach to distribution, I want you to think the first place it starts is in our vascular space. What's our vascular space? That's our blood or our plasma. And from this vascular space, it's going to our extravascular space. So what does that mean? This could be fat. This could be muscles. This could be your interstitial space, the space between your cells. And so, I'm not the best artist but let's just draw a little picture because pictures help. Let's assume this is our blood vessel so this is our vascular space. And out here is our extravascular space. What distribution is, is the process of going from our vascular space to our extravascular space. So if I had - if this was a drug, when it goes from here out there, that is distribution. Now this is a little bit different than absorption. Absorption was everything before it got to our systemic circulation. So where is absorption occurring and I'll have to cop out just a little bit and say this depends. If we take a drug orally, we're talking our GI tract. If we use an inhaler, we're talking our lungs. If we use an injection intravenously, we are you know actually not really absorbing it. We have 100% absorption. So when you think absorption, I want you to think of this depends on the route of administration. It depends on the route of administration so when you see the route of administration, think absorption. Now let's use this knowledge and apply it to something. So let's look at the title of a paper from a clinical journal and this journal is the International Journal of Antimicrobial Agents. Well, let's see if we can understand this. The title of the paper is "Pharmacokinetics of a loading dose of amikacin in septic patients undergoing continuous renal replacement therapy." Sounds tough. Let's break it down. Pharmacokinetics, we know what that means right? Pharmacokinetics is the change in concentration of a drug as it moves to the different compartments of your body. So that's really the big point of this paper. Now, of a loading dose. So a loading dose, we're kind of referring to a route of administration here and we'll talk about you know what a loading dose is but we're really dealing with absorption. And what a loading is (I'll just tell you now) is we give a higher dose of things in order to avoid a slow absorption and a slow increase in drug concentration in the plasma. So, loading dose - we're dealing with absorption - of amikacin (Amikacin is just an antibiotic) in septic patients undergoing continuous renal replacement therapy. So we see this word renal, that should be going ding, ding, ding, ding in your head. We just covered that right? When I think renal, I should be thinking what? I should be thinking excretion. So, a patient who is on continuous renal replacement therapy. What this is, is a blood filtering mechanism. Hemofiltration mechanism for patients who have renal failure. So acute renal failure. So, we know that there's probably some excretion component of pharmacodynamics that might be tested here and finally, this one is not as obvious and so, let's use a different color. Septic patients. So, when they're talking about septic patients, they're saying a patient who is in septic shock. And so, one of the things about septic shock is you get massive vasodilation, you get hypotension and what does that mean? How does that relate to what we're talking about? Well, if we think about a capillary endothelium that's been vasodilated, those individual cells are now spaced further apart than they were in the past. So what I'm drawing here is a capillary endothelium that's been vasodilated. This is our vascular space. And so, if distribution was a process of going from our vascular space to our extravascular space, can we assume that because that we have a septic patient, that might change? And the answer is yes. We have a septic patient so that's changing distribution or the process of drugs going from intravascular to extravascular. So here, the only thing missing distribution is it didn't really have anything to indicate metabolism but 3 out of those 4 components of pharmacokinetics are addressed here. Makes sense? I hope so. So before we move on to the next section, I want you to just stop, think and repeat some of the core concepts that we've covered here and do these on your own And once you've got this down, you can move on to the next section or if you're feeling adventurous, you can just move on without doing it. In the next section, what we're going to be doing is covering absorption in detail. I hope to see you there. Subtitles by the Amara.org community
Pharmacology
A study found it to bind to the cough center in the medulla oblongata, more specifically the dextromethorphan-binding site in guinea pig brain with high affinity.[3]
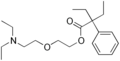
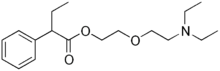
As a 2-(2-diethylaminoethoxy)ethyl ester, it is chemically related to oxeladin and pentoxyverine, which are in the same class. (Oxeladin has an additional ethyl group in its carboxylic acid, pentoxyverine has both ethyl groups of oxeladin replaced by one cyclopentyl in the same place.)
See also
- Cough syrup
- Noscapine
- Codeine; Pholcodine
- Dextromethorphan; Dimemorfan
- Racemorphan; Dextrorphan; Levorphanol
- Pentoxyverine
- Tipepidine
- Cloperastine; Levocloperastine
References
- ^ Germouty J, Weibel MA (November 1990). "[Clinical comparison of butamirate citrate with a codeine-based antitussive agent]". Revue Médicale de la Suisse Romande. 110 (11): 983–6. PMID 1980027.
- ^ a b Schlesser JL (1991). Drugs Available Abroad, 1st Edition. Derwent Publications Ltd. pp. 29–30. ISBN 0-8103-7177-4.
- ^ Klein M, Musacchio JM (October 1989). "High affinity dextromethorphan binding sites in guinea pig brain. Effect of sigma ligands and other agents". The Journal of Pharmacology and Experimental Therapeutics. 251 (1): 207–15. PMID 2477524.