| Follicular phase | |
|---|---|
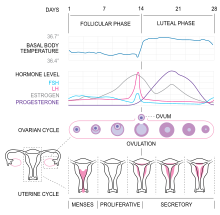 Figure 1. Menstrual cycle illustrating hormone levels, follicle development and uterine cycle | |
| Biological system | Urogenital system(reproductive) |
The follicular phase, also known as the preovulatory phase or proliferative phase,[1] is the phase of the estrous cycle (or, in primates[2] for example, the menstrual cycle) during which follicles in the ovary mature from primary follicle to a fully mature graafian follicle. It ends with ovulation. The main hormones controlling this stage are secretion of gonadotropin-releasing hormones, which are follicle-stimulating hormones and luteinising hormones. They are released by pulsatile secretion.[1] The duration of the follicular phase can differ depending on the length of the menstrual cycle, while the luteal phase is usually stable, does not really change and lasts 14 days.
YouTube Encyclopedic
-
1/5Views:385 2002 609 559570 208468 6336 354
-
Reproductive cycle graph-Follicular phase | NCLEX-RN | Khan Academy
-
The menstrual cycle
-
Understanding the Menstrual Cycle
-
Menstrual Cycle Phases | Female Reproductive System | Follicular Luteal Proliferative Secretory
-
Follicular Phase: The Egg-producing Phase
Transcription
- [Voiceover] So we know that a female's eggs develop in her ovaries and that as they sort of develop, we get these fluctuations in female sex hormones released from the ovaries. So to be more specific, we get Estrogen, we get Progesterone, and we get Inhibin released from the ovaries while the eggs are developing. So that's all fine and good, but why exactly is this happening? What exactly are these hormones doing in the female body? And why do their levels change? Well, there's this handy graph that we'll just refer to as the Ovarian Cycle Graph that I guarantee you'll see if you're studying female reproductive physiology. It's actually really quite helpful in understanding and visualizing what exactly is going on in the body during each reproductive cycle. So this is sort of the skeleton of the graph here. Just the axes. And I'll orient you to the axes first, and then we'll look at what information the graph actually contains. So the x axis here is time. And time in this situation is sorta constricted to 28 days because that's how long each reproductive cycle is. And by the way, it says "28/0" here because 28th day is the same day as the zeroeth day, if that makes sense. In other words, once you reach day 28 of one cycle, you're on day 0 of the next cycle. There's no sorta gap in between. And remember ovulation happens here at day 14. So that's the x axis. And before we talk about the y axis, I'll just quickly mention that we're gonna split the reproductive cycle into two main phases, the Follicular Phase and the Luteal Phase. And you'll see why they're called that soon. So on the y axis, there's a few different things that we'll sorta track at the same time. And the reason that they're all here on the y axis at the same time is because they're all related. They happen at the same time in the body, so we want to see them all at once on one graph. They're even listed in a sort of order on this graph. So first at the top, we've got the Gonadotrophic Hormone Levels, FSH and LH. And remember these are released from the anterior pituitary gland in the brain. And these hormones affect the development of follicles in the ovarian cycle. And these hormones affect the development of follicles in the ovarian cycle. I'll actually look at the Ovarian Cycle just below here. And as the follicles develop, they cause the release of hormones from the ovaries. So the hormone levels are here below. And last, we have stages of the Uterine Cycle, which are influenced by the levels of sex hormones released from the ovaries. And broadly, the stages of the Uterine Cycle are Menses or menstruation, where the endometrial lining is shed, the Proliferative Phase, where a new layer of endometrium forms and grows or proliferates, and the last phase is the Secretory Phase, where the endometrium becomes ready for implantation by a fertilized egg. So even if there is no fertilization of the egg, the endometrium still gets ready just in case. And we'll talk about these phases a little bit more later on. And let me just quickly say that in pink up here in the Ovarian Hormones Levels, the pink here is Estrogen, the blue line underneath it is Inhibin, and the orange-y line is Progesterone. So those are the three ovarian hormones that we're going to be concerned with. So we've got this sort of logical step-wise setup here. And hopefully that makes it easier to remember what's going on. So for now, we'll just look at the first half of the graph, the Follicular Phase part of the graph, and we won't really worry about the Luteal Phase part of the graph just yet. We'll just get rid of that. So on day 0 here, the anterior pituitary gland is releasing some FSH and some LH. And you can see those baseline levels here. And we know that the FSH is stimulating growth of the follicle here. And you can see it growing as the days go by. And while it grows, its number of granulosis cells is increasing, right? The granulosis cells are represented by this purple color here. And we know the granulosis cells secrete Estrogen. So the amount of Estrogen in the blood is going up and up and up as these follicles grow. And to add to that, besides what FSH is doing, luteinizing hormone is making the thecal cells that surround the follicle produce a hormone called Androstenedione. Androstenedione is really, really similar in structure to Estrogen. And actually the granulosis cells get a hold of that Androstenedione and convert it to actual Estrogen. So the Estrogen levels are just going way up, and you can see that reflected here. So as the follicles grow, the Estrogen level is just going way up. And by the way, if we look down here at what's happening in the endometrium of the uterus, that's the inner lining of the uterus, we can see that we're in the Proliferative Phase. And it's called the Proliferative Phase because the increasing Estrogen levels that we see here are inducing a new layer of endometrium to form since the old one was shed in menstruation in the previous week. So that's what this Proliferation Phase is all about. So at this point some really interesting stuff starts to happen. So when the hypothalamus and the anterior pituitary gland in the brain start to sense that the levels of Estrogen are super high like this, they begin to release less FSH and LH. And you can see them dipping here. And that sorta makes sense, right? Because the point of releasing FSH and LH in the first place was to cause development of the follicles. And the follicles make the Estrogen so when the brain senses lots of Estrogen, it must mean that the follicles are developing, right? So it doesn't actually have to continue to release so much FSH and LH. That makes sense. So that's why we see these dips here in FSH and LH levels in the blood because the high Estrogen levels tell the brain to sorta reduce their production and release of these gonadotrophic hormones. But then it starts to get even more interesting. Our granulosis cells are just cranking out Estrogen at this point, and they actually start to produce two more hormones in higher amounts. They start to produce a bit of Progesterone, and they start to produce a hormone called Inhibin. And let me just say that there's two types of Inhibin, Inhibin A and Inhibin B, but we're just going to consider them as one thing for now, Inhibin. And Inhibin's role is to inhibit FSH release from the anterior pituitary. So you can kinda see here that as Inhibin starts to increase, FSH in blue here starts to decrease. And again, that's because Inhibin is stopping the anterior pitutary from releasing FSH. You might think that's the end of the interesting stuff. It gets even more interesting. Do you remember how we said that as Estrogen gets higher and higher, it stops the hypothalamus and the anterior pituitary from making more FSH and LH by a bit of negative feedback? Well, it turns out that if Estrogen reaches a super high level like up here, we'll say it reaches that super high level up here, it actually causes the brain to want to release more FSH and LH. It's sort of a paradoxical sounding event. So we reach such a high level of Estrogen that the brain tries to release this really, really high amount of FSH and LH. But on the graph here we only really see a high release of LH and not FSH. So, why is that? Aha! Remember earlier we said that our granulosis cells were releasing Inhibin, which reduces FSH release from the anterior pituitary? Well, look here. Our Inhibin amount is pretty high now, and that Inhibin sorta curtails the amount of FSH released from the anterior pituitary. But it doesn't really affect the LH that gets released. So the net effect is a huge release of LH from the anterior pituitary in an event called the Luteal Surge. And this LH that gets released, plus the still reasonably high amount of FSH that gets released, that sort of pushes development of the follicle to its final step, ovulation. And the egg you can see sort of popping out of the follicle here in the process of ovulation. And remember that happens at day 14 here. So that's the Follicular Phase and ovulation on the graph.
Hormonal events
Protein secretion
Due to the increase of FSH, the protein inhibin B will be secreted by the granulosa cells. Inhibin B will eventually blunt the secretion of FSH toward the end of the follicular phase. Inhibin B levels will be highest during the LH surge before ovulation and will quickly decrease after.[1]
Follicle recruitment

Follicle-stimulating hormone (FSH) is secreted by the anterior pituitary gland (Figure 2). FSH secretion begins to rise in the last few days of the previous menstrual cycle,[3] and is the highest and most important during the first week of the follicular phase[4] (Figure 1). The rise in FSH levels recruits five to seven tertiary-stage ovarian follicles (this stage follicle is also known as a Graafian follicle or antral follicle) for entry into the menstrual cycle. These follicles, that have been growing for the better part of a year in a process known as folliculogenesis, compete with each other for dominance.[5]
FSH induces the proliferation of granulosa cells in the developing follicles, and the expression of luteinizing hormone (LH) receptors on these granulosa cells (Figure 1). Under the influence of FSH, aromatase and p450 enzymes are activated, causing the granulosa cells to begin to secrete estrogen. This increased level of estrogen stimulates production of gonadotropin-releasing hormone (GnRH), which increases production of LH.[4] LH induces androgen synthesis by thecal cells, stimulates proliferation, differentiation, and secretion of follicular thecal cells and increases LH receptor expression on granulosa cells.[4]
Throughout the entire follicular phase, rising estrogen levels in the blood stimulates growth of the endometrium and myometrium of the uterus.[6] It also causes endometrial cells to produce receptors for progesterone,[6] which helps prime the endometrium to respond to rising levels of progesterone during the late proliferative phase and throughout the luteal phase.
Estrogen surge
Two or three days before LH levels begin to increase,[7] usually by day seven of the cycle,[8] one (or occasionally two) of the recruited follicles has emerged as dominant. Many endocrinologists believe that the estrogen secretion of the dominant follicle has increased to a level that GnRH production is suppressed, which lowers the levels of LH and FSH. This slowdown in LH and FSH production leads to the atresia (death) of most of the recruited follicles, though the dominant follicle continues to mature. Estrogen levels will continue to increase for several days (on average, six days, but this varies widely).[7]
These high estrogen levels initiate the formation of a new layer of endometrium in the uterus, histologically identified as the proliferative endometrium. Crypts in the cervix are also stimulated to produce fertile cervical mucus.[7] This mucus reduces the acidity of the vagina, creating a more hospitable environment for sperm.[9] It also has a characteristic texture that helps guide sperm through the cervix[10] and to the fallopian tubes, where they wait for ovulation.[medical citation needed] In addition, basal body temperature may lower slightly under the influence of high estrogen levels.[11]
LH surge and ovulation
Estrogen levels are highest right before the LH surge begins (Figure 1). The short-term drop in steroid hormones between the beginning of the LH surge and the event of ovulation may cause mid-cycle spotting or bleeding.[12] Under the influence of the preovulatory LH surge, the first meiotic division of the oocytes is completed. The surge also initiates luteinization of thecal and granulosa cells.[4] Ovulation normally occurs 30 (± 2) hours after the beginning of the LH surge (when LH is first detectable in urine).[13]
Follicular waves
Follicular waves are best described as the phase when follicles have matured sufficiently and rupture, leading to ovulation. Recent findings into the menstrual cycle in mammals has discovered that 2 or more follicles can develop but only one of the follicles fully matures to release the egg.[14][15] This follicular wave involves multiple surges in the levels of FSH to initiate follicular development. A study has found that 68% of women tended to display two follicular wave developments before ovulation while the remaining had three waves.[16]
References
- ^ a b c Carol N. Monis; Maggie Tetrokalashvili. (2019). "Menstrual Cycle Proliferative And Follicular Phase". Treasure Island (FL): StatPearls Publishing. PMID 31194386.
 This article incorporates text available under the CC BY 4.0 license.
This article incorporates text available under the CC BY 4.0 license.
- ^ "Primate | Definition, Biology, & Facts | Britannica". 3 January 2024.
- ^ Reed, Beverly G.; Carr, Bruce R. (2000). "The Normal Menstrual Cycle and the Control of Ovulation". In De Groot, Leslie J.; Chrousos, George; Dungan, Kathleen; Feingold, Kenneth R.; Grossman, Ashley; Hershman, Jerome M.; Koch, Christian; Korbonits, Márta; McLachlan, Robert (eds.). Endotext. South Dartmouth (MA): MDText.com, Inc. PMID 25905282.
- ^ a b c d Dee Unglaub Silverthorn (2004). Human physiology: an integrated approach (Third ed.). San Francisco: Pearson/Benjamin Cummings. Chapter 26: Reproduction and Development, and Chapter 23 Endocrine control of growth and metabolism. ISBN 0-13-102015-3.
- ^ McGee, E.A., & Hsueh, A.J. (2000). Initial and cyclic recruitment of ovarian follicles. Endocrine Reviews, 200-214, 21(2). doi: 10.1210/edrv.21.2.0394
- ^ a b Strang, Eric P. Widmaier, Hershel Raff, Kevin T. (2006). Vander's human physiology the mechanisms of body function (10th ed.). Boston: McGraw-Hill. p. 678. ISBN 0-07-111677-X.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ a b c Weschler, Toni (2002). Taking Charge of Your Fertility (Revised ed.). New York: HarperCollins. pp. 359–361. ISBN 0-06-093764-5.
- ^ Stenchever Droegemuller Herbst Mishell (2001). Comprehensive Gynecology (Fourth ed.). St. Louise, Missouri: Mosby. p. 87. ISBN 0-323-01402-X.
- ^ Weschler (2002), p.57
- ^ Weschler (2002), illustrations p.59 and p.3 of color insert
- ^ Weschler (2002), pp.54,306,310
- ^ Weschler (2002), p.65
- ^ Susan B. Bullivant; Sarah A. Sellergren; Kathleen Stern; et al. (February 2004). "Women's sexual experience during the menstrual cycle: identification of the sexual phase by noninvasive measurement of luteinizing hormone". Journal of Sex Research. 41 (1): 82–93. doi:10.1080/00224490409552216. PMID 15216427. S2CID 40401379.
- ^ Evans, A. C.; Duffy, P.; Hynes, N.; Boland, M. P. (February 2000). "Waves of follicle development during the estrous cycle in sheep". Theriogenology. 53 (3): 699–715. doi:10.1016/S0093-691X(99)00268-X. ISSN 0093-691X. PMID 10735037.
- ^ Boer, H. M. T.; Röblitz, S.; Stötzel, C.; Veerkamp, R. F.; Kemp, B.; Woelders, H. (December 2011). "Mechanisms regulating follicle wave patterns in the bovine estrous cycle investigated with a mathematical model". Journal of Dairy Science. 94 (12): 5987–6000. doi:10.3168/jds.2011-4400. ISSN 1525-3198. PMID 22118087.
- ^ Baerwald, Angela R.; Adams, Gregg P.; Pierson, Roger A. (2003-09-01). "Characterization of Ovarian Follicular Wave Dynamics in Women1". Biology of Reproduction. 69 (3): 1023–1031. doi:10.1095/biolreprod.103.017772. ISSN 0006-3363. PMID 12748128.
